The Importance of Early Detection
Early detection is critical in managing dengue fever effectively. When diagnosed early, healthcare providers can initiate appropriate treatment promptly, preventing the disease from progressing into a severe form. Conversely, late diagnosis can lead to complications and increase the risk of severe illness.
Late diagnosis of dengue fever can result in the development of a disease known as dengue haemorrhagic fever (DHF) or dengue shock syndrome (DSS). DHF is characterised by bleeding, organ impairment, and, in severe cases, shock, while DSS is characterised by an immediate drop in blood pressure, which leads to organ failure and even death. These complications can be life-threatening, highlighting the urgent need for early detection.
Healthcare providers can closely monitor the patient’s condition, provide appropriate medical care, and implement preventive measures to avoid complications by identifying dengue fever in its early stages. Early detection can also facilitate the implementation of mosquito control measures in the patient’s vicinity, preventing further transmission of the virus.
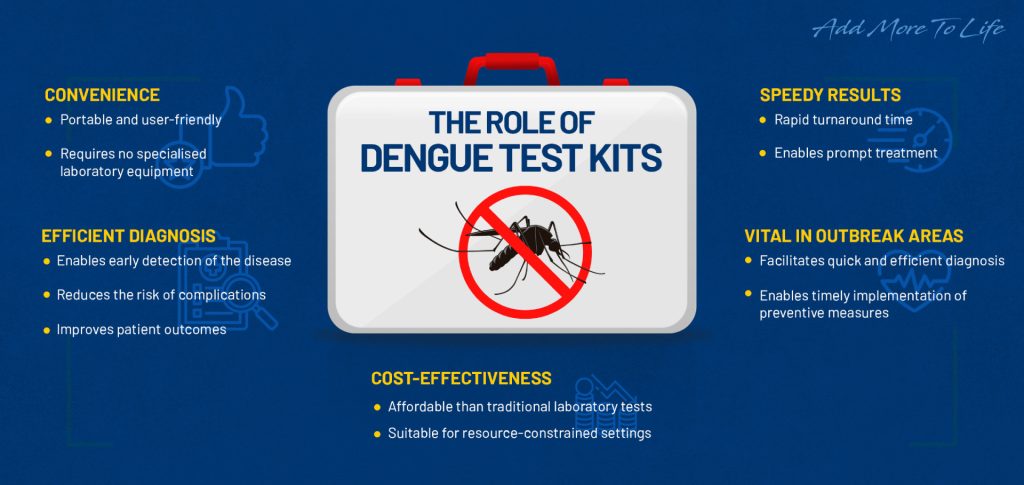
The Role of Dengue Test Kits in Early Detection
Dengue test kits are diagnostic tools designed to detect the presence of dengue virus antigens or antibodies in a patient’s blood sample. These kits offer several advantages over traditional laboratory tests, making them an invaluable tool in early detection.
- Convenient and Portable : Compared to traditional laboratory tests, dengue test kits are more convenient. In addition, they are usually portable and can be used at clinics or hospitals, enabling healthcare providers to obtain rapid results without needing specialised laboratory equipment. This convenience is especially crucial in areas with limited access to well-equipped laboratories, allowing for quick and efficient diagnosis
- Speedy Results : Another advantage of dengue test kits is the speed at which results can be obtained. While traditional laboratory tests may take several hours or even days to yield results, dengue test kits can provide results within minutes. This rapid turnaround time allows healthcare providers to initiate appropriate treatment promptly, reducing the risk of complications and improving patient outcomes.
- Cost-Effective : Moreover, dengue test kits are more cost-effective compared to traditional laboratory tests. The affordability and accessibility of these kits make them suitable for widespread use in areas with limited healthcare resources, facilitating early detection even in resource-constrained settings.
Interpreting the Results
Understanding how to interpret the results of dengue test kits is crucial in determining the appropriate course of action.
A positive result on a dengue test indicates the presence of dengue virus antigens or antibodies in the patient’s blood. This confirms the diagnosis of dengue fever, indicating an active infection. In such cases, healthcare providers can implement appropriate treatment measures, closely monitor the patient’s condition, and provide necessary supportive care.
In addition to medical management, preventive measures should be implemented to reduce the risk of further transmission. For example, patients diagnosed with dengue fever should adopt precautionary measures to prevent mosquito bites, such as protective clothing, insect repellents, and eliminating stagnant water sources where mosquitoes breed.
On the other hand, a negative result suggests the absence of dengue virus antigens or antibodies in the blood sample. However, it is essential to remember that a negative result obtained within the first few days of symptom onset does not rule out dengue infection completely. It is recommended to retake the test after a few days to confirm the absence of the virus.
Conclusion
Early detection is pivotal in effectively managing dengue fever and preventing complications. Timely diagnosis allows healthcare providers to initiate appropriate treatment, closely monitor the patient’s condition, and implement preventive measures to minimise the risk of severe illness.
Through a combination of early detection, proper medical care, and preventive measures, we can work towards reducing the impact of dengue fever and protecting the health and well-being of individuals in affected regions worldwide.
FAQs
Q: How does early detection of dengue fever contribute to preventing severe complications?
A: Early detection allows healthcare providers to initiate prompt treatment, closely monitor the patient’s condition, and implement preventive measures. By intervening early, the risk of the disease progressing into severe forms such as dengue haemorrhagic fever (DHF) or dengue shock syndrome (DSS) is minimised, reducing the chances of organ impairment, bleeding, and shock.
Q: What are the advantages of using dengue test kits compared to traditional laboratory tests?
A: Dengue test kits offer several advantages over traditional laboratory tests. They are easier to use and can be used without needing specialised laboratory equipment. Additionally, they provide faster results, often within minutes, enabling healthcare providers to take immediate action. Moreover, dengue test kits are more cost-effective, making them accessible in resource-limited settings where traditional laboratory tests may be less feasible.
Q: How can the results of dengue test kits be interpreted?
A: Interpreting the results of dengue test kits is essential for determining the next course of action. A positive result indicates the presence of dengue virus antigens or antibodies, confirming an active infection. In such cases, healthcare providers can implement appropriate treatment and closely monitor the patient’s condition. Conversely, a negative result suggests the absence of the virus. However, it should be noted that a negative result obtained within the first few days of symptom onset does not rule out dengue infection completely, and the test may need to be repeated.
Q: What should be done after receiving a positive result from a dengue test kit?
A: After a positive result, following healthcare providers’ instructions for further management is crucial. This may involve rest, fluid intake, and symptomatic relief medications. Monitoring for any signs of complications is essential, and preventive measures to avoid mosquito bites should be implemented. Close communication with healthcare providers and adherence to their recommendations is vital to managing the disease effectively.
Q: How do dengue test kits contribute to combating dengue fever on a larger scale?
A: Dengue test kits significantly combat dengue fever by enabling early detection, especially in areas with limited healthcare resources. Their portability, rapid results, and cost-effectiveness make them valuable tools in identifying cases early, facilitating prompt treatment, and implementing preventive measures. By employing these kits widely, the impact of dengue fever can be reduced, protecting the health and well-being of individuals in affected regions worldwide.