There’s no doubt that when one starts thinking about weight loss surgery, he or she is looking way ahead to the results, pain, and life after the surgery. It is important to accept that any surgery, in general, will have some kind of pain associated and patients should accept it as a part of the process. And especially after bariatric surgery, it’s very common for any patient to experience stomach pain. Weight loss surgery is considered major surgery and, to varying degrees, it is usual to experience a range of symptoms. These may include nausea, heartburn, GERD, uncontrollable vomiting, sleeplessness, surgical pain, fatigue, light-headedness, gas pain, pain in the left shoulder, and emotional ups and downs in the early days and weeks after surgery. Up to 30% of patients experience some sort of abdominal pain after undergoing bariatric surgery. Mostly, the abdominal pain is due to the body, particularly the stomach, coping up with the surgery, and can be encountered, if one accidentally overeats. Apart from pain, patients also suffer from other abdominal symptoms, depending upon their history and the surgery procedure. Post-bariatric surgery, one will have a feeling of fullness, after eating much less food, as compared to an ordinary person. The feeling of fullness after the surgery is much like a nauseating feeling, feeling after over-eating, otherwise. One will be able to cope up with this pain, gradually as they self-adjust their meal portions to much lesser quantities.
On the other hand, it is just not about the pain and accompanying symptoms of bariatric surgery, one must also be well aware of certain risk factors associated with the surgery. And, it goes without saying that as with any major abdominal surgery, there are risks associated with bariatric surgery too and surgery should not be considered unless you and your surgeon evaluate all other possible options. An ideal approach to weight-loss surgery requires proper discussion and careful consideration of all the associated risk factors (Short-term/ Long-term). But, surgery with proper aftercare and adequate lifestyle changes can bring astounding long-term results for health and weight.
The safest form of a Weight-loss Surgery



We all know that obesity is a major health problem worldwide, and various forms of surgeries aim to shrink the stomach and affect nutrition absorption to help the patient lose weight. Bariatric surgery is considered to be the most substantial and constant weight loss solution for obese patients. But patients should consider this surgery only after exploring all other options for weight loss like dieting, exercise, and drug treatments. Currently, there are 4 standard surgeries for weight loss and they are as follows
Gastric bypass: This surgery is restrictive/malabsorptive and involves two procedures. A small pouch is created by stapling the stomach and then the small intestine is cut and the lower part is attached to the pouch, bypassing a major part of the stomach.
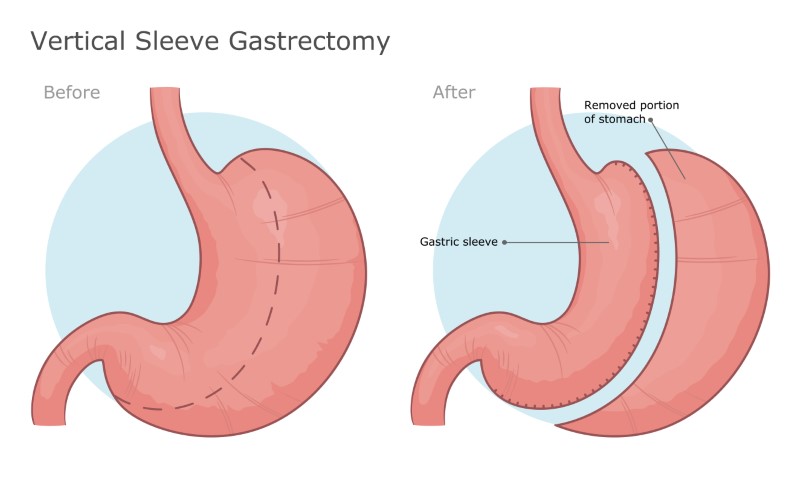
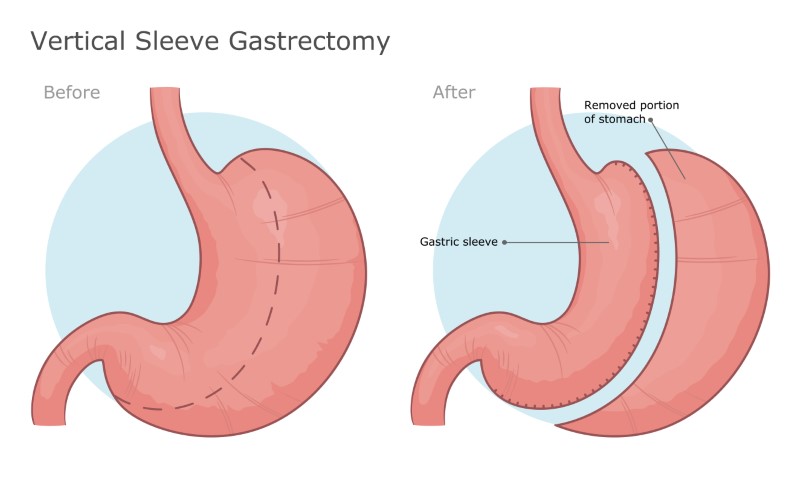
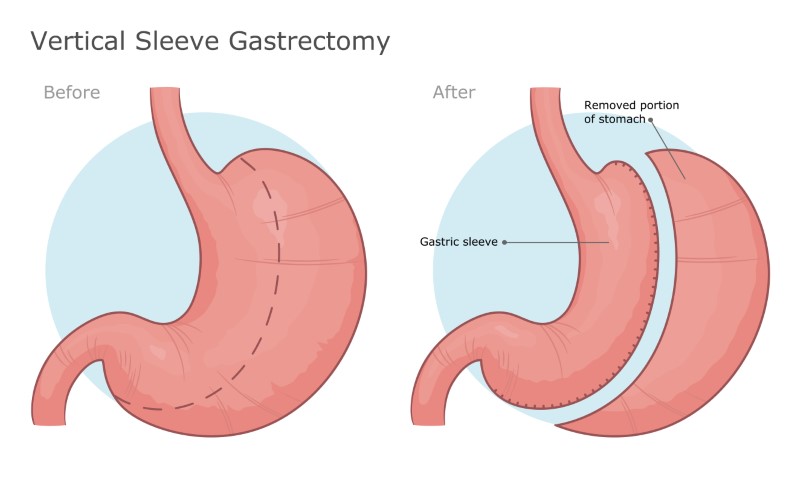
Gastric sleeve or sleeve gastrectomy: This is a restrictive laparoscopic surgery in which about 75% to 85% of the stomach is removed and only a small portion is stapled. This reduces the quantity of food intake and does not affect the absorption of nutrients.
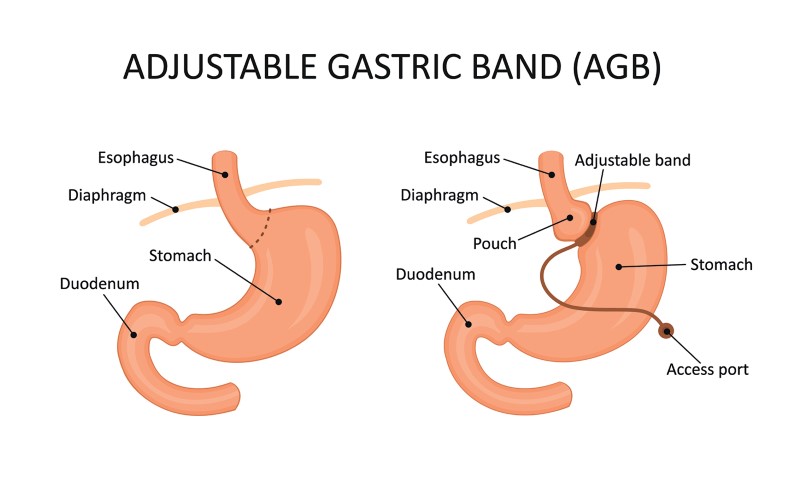
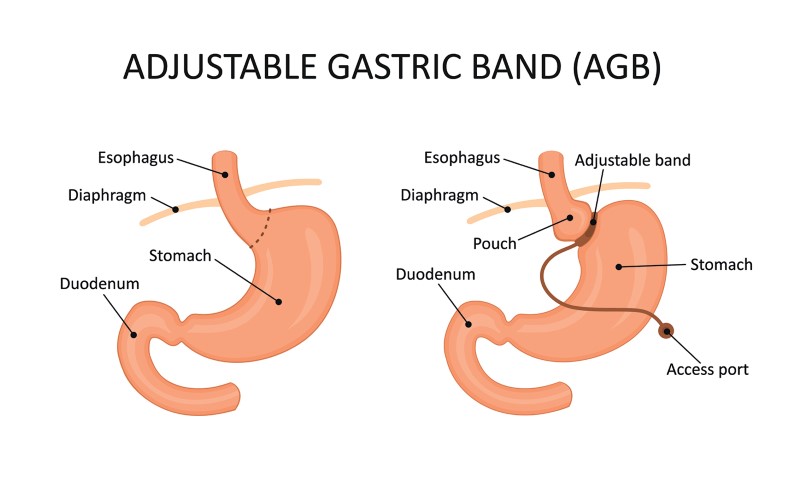
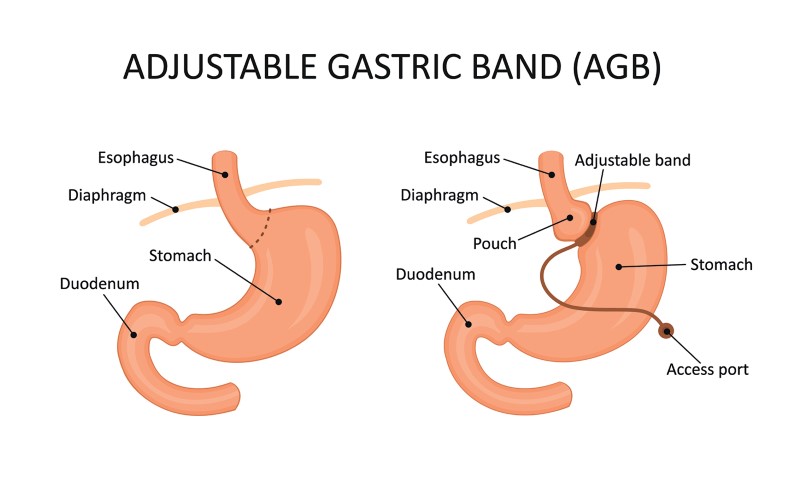
Adjustable gastric banding: This again is a restrictive surgery in which the surgeon places an inflatable band over the top portion of the stomach which divides the stomach into two sections, creating a small pouch on top of the main stomach, connected to it by a small channel. This slows down the passage of food that goes into the main stomach eventually reducing the overall intake.
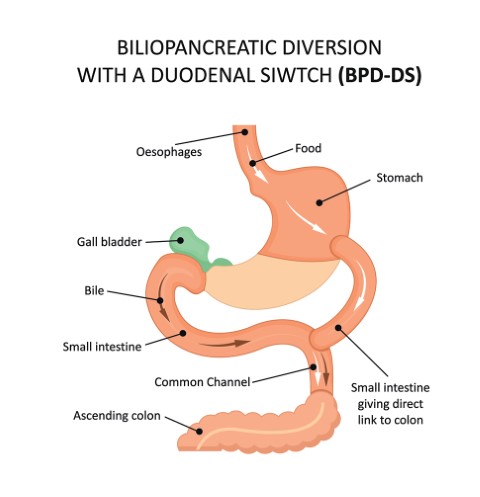
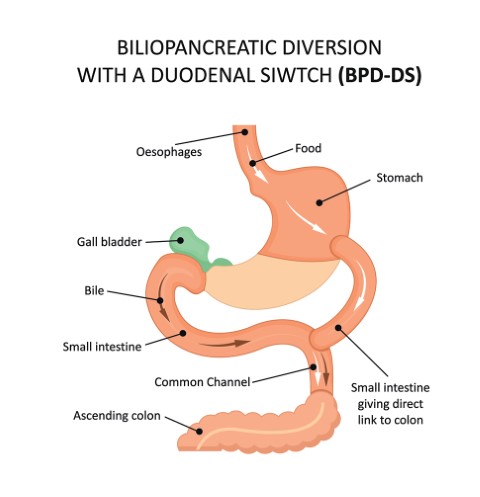
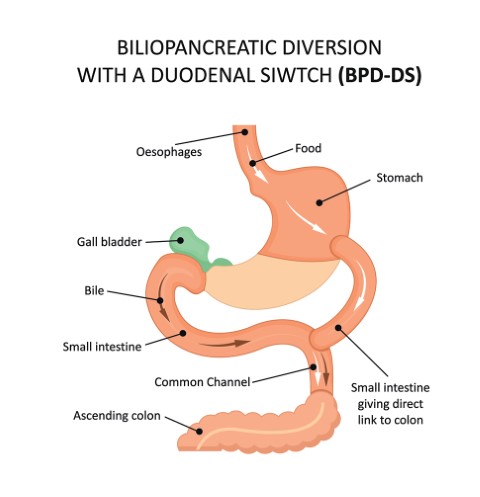
Biliopancreatic diversion with duodenal switch: This is a restrictive/malabsorptive surgery performed in two standard steps. Firstly, a sleeve gastrectomy is performed in which most of the stomach is removed and is connected to the pouch to the end of the small intestine bypassing most of it.
Each type of bariatric surgery comes with its positives and negatives. Some offer rapid initial weight loss, some are minimally invasive, and few might require minimum post-operative care. Just like the pros, there are also certain cons related to these surgeries like nutritional deficiencies, permanent and irreversible results, and slow weight loss rate in some cases. It is completely dependent on the surgeon to suggest the type of surgery basis a detailed evaluation of the patient’s BMI, health parameters, and personal needs. But, regardless of the approach, every type of bariatric surgery result in significant weight loss.
What to expect after weight loss surgery?
Usually, one can expect a significant weight loss (up to 60%) after the surgery. Also, a significant improvement is observed in other conditions such as your blood sugar levels, high blood lipid levels or sleep disorders, which are related to higher body weight. This indirectly impacts the quality of life and enhances it. But, don’t think that these improvements will be permanent. You will be required to follow certain healthy lifestyle recommendations after surgery to avoid regaining the lost weight. Eating small and frequent meals becomes an essential part of the recovery phase as eating large meals can create problems for the small-sized stomach. Ask a dietitian to help you create a plan that will get you all the nutrients you need and top it up with a good workout regime that focuses on managing weight and improving muscle growth that can help you in a quicker return to a healthier lifestyle. Remember to stay in touch with your medical team and to attend all follow-up appointments that are scheduled as part of your recovery. Also, keep a personal check on your progress and don’t hesitate to contact your primary care doctor if any medical concerns arise.






