What if we could catch a major women’s health threat early enough to truly make a difference? Today, we are championing a cause that could change the course of many lives by empowering every woman to take control of her health through regular ovarian cancer screening. As we explore this critical topic, let’s uncover how accessible and essential health practices can help detect this silent killer early.
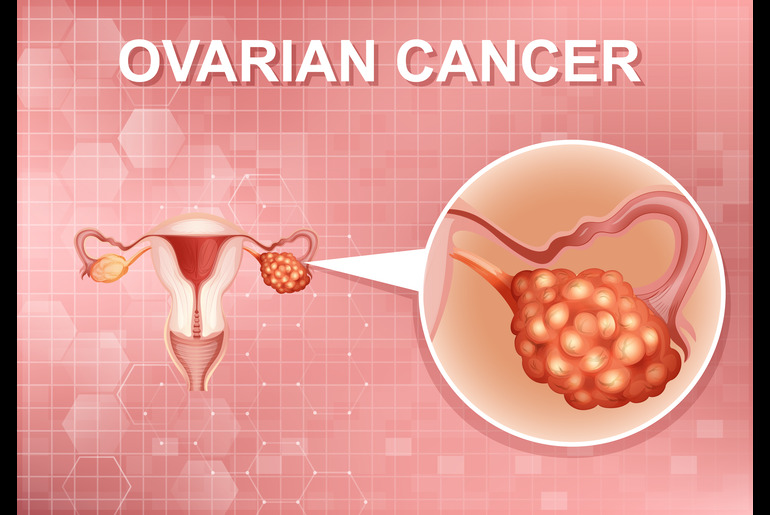
What is Ovarian Cancer?
Ovarian cancer begins in the ovaries, which is where the eggs are produced. This cancer often goes unnoticed in its early stages because it typically doesn’t show many clear or specific symptoms, which can make it hard to detect early. When symptoms like bloating, pelvic pain, and changes in bathroom habits do occur, they often resemble common stomach and digestive issues, leading many to overlook them until the cancer has progressed. As per the World Cancer Research Fund, globally, ovarian cancer is the eighth most common cancer in women.
Types of Ovarian Cancer Screening
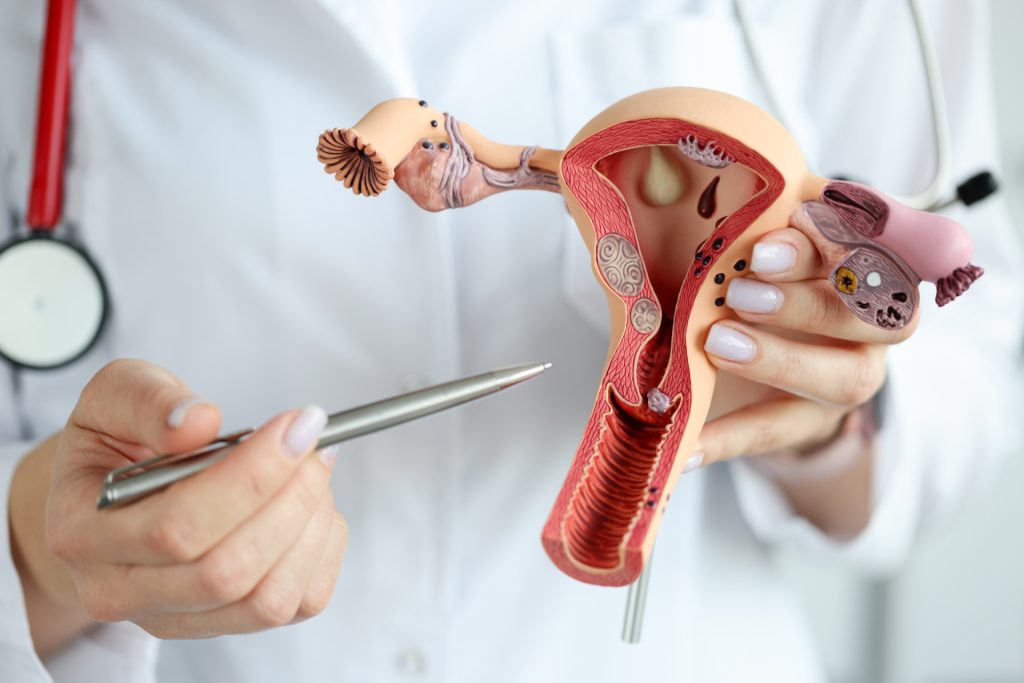
Screening for ovarian cancer typically involves methods designed to detect cancer before symptoms become apparent. The most common screenings include the transvaginal ultrasound (TVUS) and the CA-125 blood test. TVUS is a type of pelvic ultrasound used extensively to examine the reproductive organs and detect anomalies in the ovaries. Meanwhile, the CA-125 blood test measures the level of the protein CA-125, which is often elevated in women with ovarian cancer.
Who is Eligible for Ovarian Cancer Screening?
The following groups of women are recommended to undergo regular screenings based on their risk levels:
Women with Genetic Predispositions: Those who have a family history of ovarian, breast, or colorectal cancer should consider starting screening earlier and more frequently. This group may benefit from annual screenings starting from the age of 30 or 10 years earlier than the youngest age at the diagnosis in the family, whichever comes first.
Women with a Personal History of Cancer: Those who have previously had breast, uterine, colon, or rectal cancer often have a higher risk of developing ovarian cancer and should discuss their screening schedule with their healthcare provider.
Postmenopausal Women: Older women, especially those who have gone through menopause, are at a higher risk for ovarian cancer. They should discuss the feasibility and timing of screenings like TVUS and CA-125 blood tests with their healthcare professionals.
Regular Interval Discussions: For those who are at increased risk, discussing the appropriate intervals for screening with their healthcare provider is crucial. Generally, annual screenings are recommended, but the frequency may increase based on individual risk assessments and the advice of their healthcare provider.
Overcoming Barriers to Screening
Despite the availability of screening methods, various barriers deter women from undergoing regular ovarian cancer screenings. Lack of awareness about the disease and its screening options tops the list, followed by psychological barriers such as fear of diagnosis. Cultural beliefs and societal norms also play a significant role, where discussing gynecological health may be taboo or stigmatized. Moreover, in regions where healthcare is not readily accessible or affordable, even willing individuals may find it challenging to seek help.
Empowering women to overcome these hurdles involves a multifaceted approach. Raising awareness through community education, creating supportive environments that respect cultural sensitivities, and enhancing access to healthcare services are vital steps. Additionally, encouraging open conversations about gynecological health and normalizing these discussions can significantly reduce stigma and promote a more proactive attitude towards health screening.
Importance of Advocacy and Education
The role of advocacy and education in enhancing awareness about ovarian cancer cannot be overstated. By informing women about the importance of early screening and its potential to save lives, we can shift the narrative from fear and ignorance to empowerment and action. Advocates and educators can influence public health policies, improve healthcare services, and ensure that every woman understands the risks and the benefits of early detection.
Wrapping It Up
Let us renew our commitment to ensuring no woman is left behind in the fight against ovarian cancer. Through increased understanding, accessible screening, overcoming societal barriers, and strong advocacy, we can make a significant difference. Every woman must be empowered to take charge of her health by making ovarian cancer screening a priority.
Reference Links:
https://www.wcrf.org/cancer-trends/ovarian-cancer-statistics/
https://www.cdc.gov/cancer/ovarian/basic_info/screening.htm
https://www.mayoclinic.org/tests-procedures/ca-125-test/about/pac-20393295#:~:text=Overview,high%20risk%20of%20the%20disease.
https://ocrahope.org/get-the-facts/statistics/#:~:text=Ovarian%20cancer%20accounts%20for%202.5,the%20deadliest%20of%20gynecologic%20cancers.
https://pubmed.ncbi.nlm.nih.gov/33620837/#:~:text=Ovarian%20cancer%20is%20the%20leading,poor%20outcomes%20of%20this%20disease.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459072/
https://www.cancer.org/cancer/types/ovarian-cancer/detection-diagnosis-staging/detection.html
https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/getting-diagnosed/screening
https://www.uptodate.com/contents/screening-for-ovarian-cancer-beyond-the-basics#:~:text=In%20this%20group%2C%20ovarian%20cancer,125%20and%20a%20pelvic%20ultrasound.