Introduction
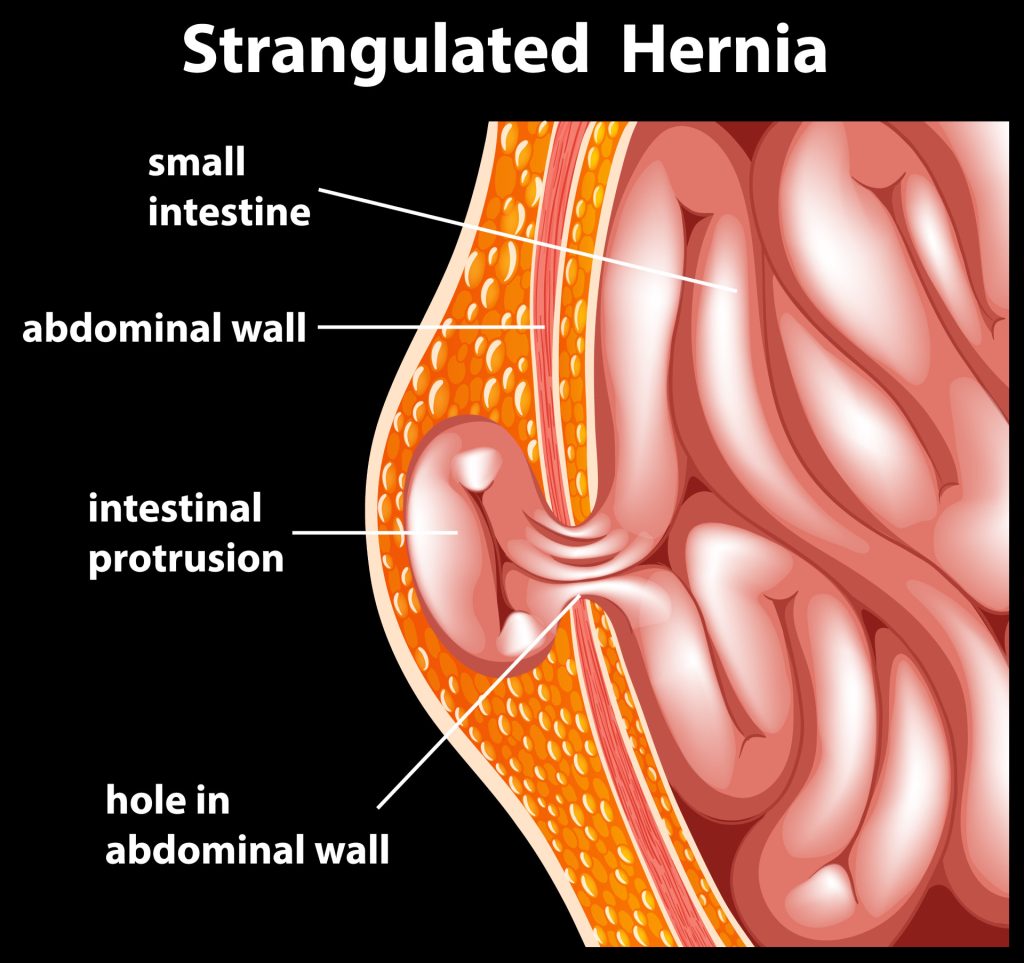
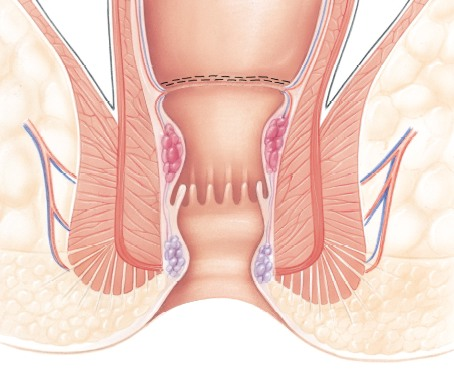
Hernias are a prevalent health condition that impacts millions of individuals globally. This medical condition happens when an internal organ or tissue protrudes through a vulnerable area in the muscle or tissue wall that encircles it. Hernias usually occur in the abdomen or the groin. They are often caused by ageing, strain, injury, or genetics. Hernias are formed by the lining of the abdomen cavity in the form of a sac, bulging out through an abnormal opening. In the past, open hernia surgery was the standard surgical option for treating hernias. However, with advancements in surgical technology, laparoscopic hernia repair has become increasingly popular. This blog will discuss the differences between open and laparoscopic hernia repair to help you decide the best surgical option.
Open versus Laparoscopic Hernia Repair:
Open hernia repair, or open surgical repair, involves a large incision (cut) in the skin and muscle to access and repair the hernia. During the procedure, the hernia sac is carefully pushed back into the abdomen, and the weakened or damaged area of the muscle or tissue wall is repaired or reinforced. After the repair, the incision is closed with stitches or surgical staples. Open hernia repair is done under local anesthesia.
Laparoscopic hernia repair, or minimally invasive, is a newer surgical procedure or option involving making a few small incisions in the abdomen instead of one large incision to repair or remove the hernia sac. A laparoscope is a thin tube with a camera and light attached that is inserted through one of the incisions. Using a laparoscope, the surgeon can view the inside of the abdomen. Additional incisions are made to insert the surgical instruments. The hernia sac is removed or pushed back into the abdomen depending on the need. The weakened or damaged area of the muscle or tissue wall is repaired or reinforced through one of the incisions. The incisions are closed with sutures. Laparoscopic hernia repair is done under general anesthesia
Advantages of Open Hernia Repair
- Suitable for all types of hernias: Open hernia repair can treat all hernias, including inguinal, umbilical, incisional, and femoral hernias.
- Straightforward procedure: The procedure is straightforward and can be performed quickly.
- No specialised equipment needed: Open hernia repair does not require any specialised equipment, making it accessible to more patients.
- Local anesthesia: Since open hernia repair is performed under local anesthesia, it is suitable for patients experiencing complications associated with general anesthesia risks.
Advantages of Laparoscopic Hernia Repair
- Shorter recovery time: The recovery time for laparoscopic hernia repair is typically shorter than open hernia repair, as the small incisions take less time to heal. You can return to everyday life and activities sooner.
- Less discomfort: Laparoscopic hernia repair causes less discomfort than open hernia repair, as the incisions are smaller and require less healing time.
- Reduced scarring: The small incisions result in minimal scarring, which can be less unsightly for better cosmetic results and less discomfort. It also removes excess tissue and tightens the skin where the hernia is.
Disadvantages of Open Hernia Repair
Despite its effectiveness, there are several disadvantages associated with this procedure.
- Longer recovery time: Open hernia repair requires a longer recovery time than laparoscopic hernia repair due to the larger incision and the need for the body to heal.
- More pain and discomfort: Patients typically experience more pain and discomfort following open hernia repair due to the larger incision and the need for a more extended recovery period.
- Scarring: The large incision can result in significant scarring, which can be unsightly and cause discomfort. Open hernia repair leaves a noticeable scar due to the large incision.
- Risk of complications: Complications such as infection, bleeding, and blood clots are potential risks with any surgery.
- Reduced mobility: Open hernia repair may reduce mobility and physical activity during recovery, potentially impacting daily activities and work.
Disadvantages of Laparoscopic Hernia Repair
Despite its many benefits, Laparoscopic hernia repair also has several disadvantages.
- Longer operating time: Laparoscopic surgery typically takes longer than traditional open surgery due to the need for precise and delicate movements of the instruments.
- Specialised equipment needed: Laparoscopic hernia repair requires specialised equipment, which may not be available at all medical facilities.
- Technical difficulties: Laparoscopic surgery can be technically challenging, with the surgeon getting restricted movement to perform the surgery through tiny incisions.
- Risk of complications: Although rare, there is a risk of complications during laparoscopic surgery, such as injury to surrounding organs, infection, bleeding, and blood clots.
- Limited use: Laparoscopic surgery is unsuitable for all types of hernias and may be ineffective for repairing larger or more complex injuries.
- Conversion to open surgery: In some cases, the surgeon may need to convert laparoscopic surgery into an open surgery, which involves a larger incision, due to complications during the procedure or difficulty in visualising the damaged area.
Conclusion
In conclusion, both open and laparoscopic hernia repair have advantages and disadvantages. Open hernia repair is a straightforward procedure that can be performed quickly and is suitable for all types of hernias. However, it has a longer recovery time, more discomfort, and can result in significant scarring. Laparoscopic hernia repair has a shorter recovery time, less discomfort, and reduced scarring. However, it requires specialised equipment and may not be suitable for all types of hernias. The best surgical option for you depends on your circumstances, pain threshold, and doctor’s recommendation. Discussing your options with your doctor and making an informed decision that is best for you is important.
FAQs :
Q. How is open hernia repair different from laparoscopic hernia repair?
Open hernia repair involves a large incision in the skin and muscle to access and repair the hernia. In contrast, laparoscopic hernia repair involves several small incisions in the skin and using a laparoscope to repair the hernia.
Q. Which is better, open or laparoscopic hernia repair?
The best surgical option for you depends on your circumstances and the doctor’s recommendation. Both open and laparoscopic hernia repair have advantages and disadvantages, and your doctor will help you make an informed choice based on your specific needs.
Q. Is laparoscopic hernia repair less painful than open hernia repair?
Typically, laparoscopic hernia repair is less painful than open hernia repair as the incisions are smaller and take less time to heal. However, the level of discomfort and pain can vary from person to person.
Q. Is laparoscopic hernia repair a newer procedure compared to open hernia repair?
Yes, laparoscopic hernia repair is a newer surgical option than open hernia repair. It has only become popular with advancements in surgical technology.
Q. Is laparoscopic hernia repair more expensive than open hernia repair?
The cost of laparoscopic hernia repair may be higher than open hernia repair, as it requires specialised equipment. However, the cost can vary depending on location, insurance coverage, and other factors.
Q. Is the recovery time shorter after laparoscopic hernia repair than after open hernia repair?
Typically, the recovery time after laparoscopic hernia repair is shorter than open hernia repair, as the small incisions take less time to heal. However, the recovery time can vary from person to person.