Introduction
Coronary artery disease (CAD) is a serious condition that affects millions of people around the world. It is a form of cardiovascular disease that is caused by the hardening and narrowing of the arteries that supply blood to the heart. If left untreated, coronary artery disease (CAD) lead to chest pain, complete blockage of an artery, heart attack, and cause sudden death. Knowing the symptoms, risk factors, and treatments for CAD can help you protect yourself and those around you from its potentially devastating effects. In this article, we’ll explore what you need to know about coronary artery disease and how to identify and manage this devastating condition and keep it at bay. However, there are also various preventative measures that you can take to reduce your risk of developing the condition. With the right information and knowledge, you can reduce your risk of developing this dangerous condition and improve your overall heart health.
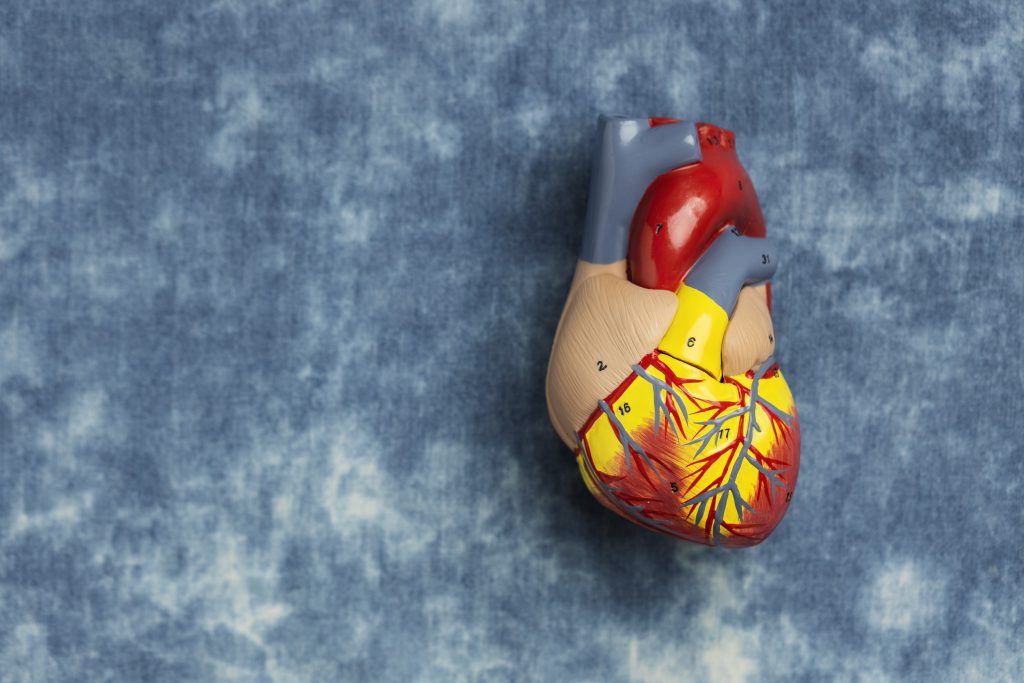
What is coronary artery disease?
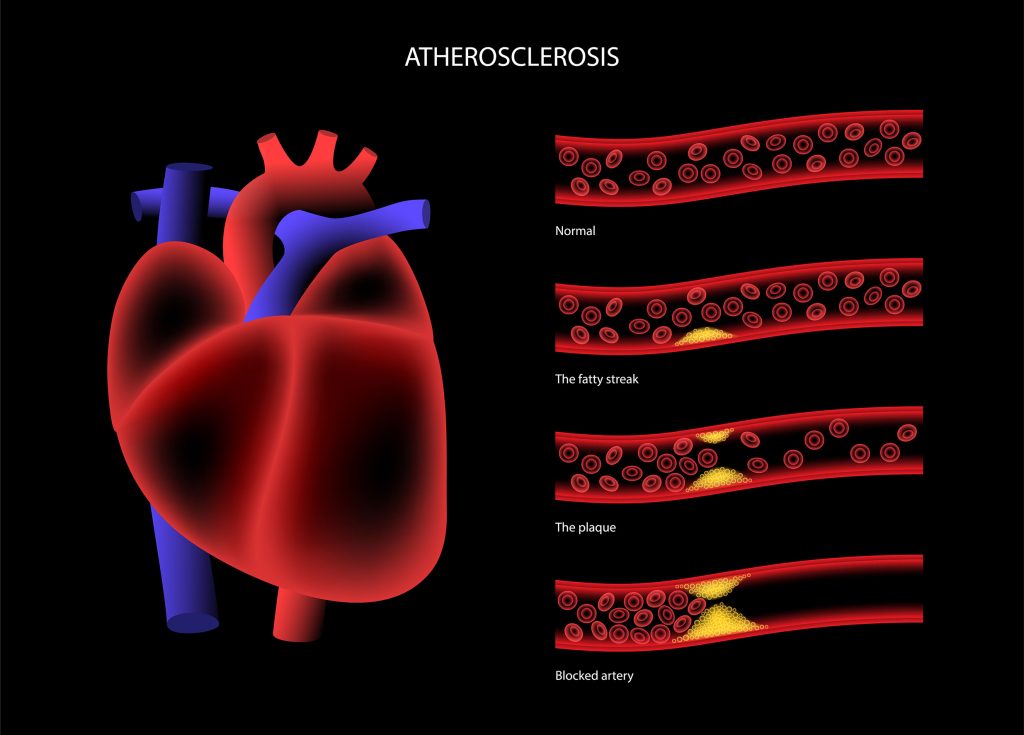
Coronary artery disease (CAD) is a medical condition in which plaque builds up in the arteries that supply blood to your heart. The buildup of fatty deposits in the arteries is a common precursor to CAD, this build-up of fatty deposits in the arteries could be formed over a period of time, which can completely block the arteries and cause heart failure. This buildup causes the arteries to narrow, which increases your risk of a heart attack. The plaque that builds up in the arteries can be made of cholesterol, calcium, and pieces of fatty material. It usually starts in the walls of the arteries, and it can build up and grow bigger over time, which puts pressure on the artery walls. This can make it harder for your heart to get the blood it needs. In most cases, CAD is the result of a combination of risk factors that increase your chances of developing it. These risk factors include aging, smoking, high blood pressure, high cholesterol, diabetes, and obesity. While these risk factors can be controlled with lifestyle changes, there are treatments that can help reduce your risk of developing CAD.
Symptoms of coronary artery disease
The first and most common symptom of CAD is chest pain. The pain may feel like pressure, squeezing, or an achy and heavy feeling in your chest. It can be mild or severe, and it can feel like something is pressing on your chest or that it’s hard to breathe. Other symptoms of CAD can include
- shortness of breath,
- weakness or fatigue,
- dizziness or lightheadedness
- palpitations,
- pain or pressure in your shoulders or arms,
- nausea or vomiting,
- sweating,
- fainting.
If you experience any of these symptoms, it’s important to see your doctor. The sooner you get treatment, the better your chances are of preventing a heart attack and reducing your risk of mortality.
Risk factors of coronary artery disease
As mentioned above, most cases of CAD are caused by a combination of risk factors. These factors may include aging, smoking, high blood pressure, high cholesterol, diabetes, and obesity. Depending on your individual risk level, these risk factors can lead to CAD in two ways: They can cause the buildup of plaque in the arteries, or they can increase your risk of blood clots forming in the arteries.
Diagnosis of coronary artery disease
If your doctor suspects that you have CAD, they would advise on heart health evaluation tests to diagnose further. This includes a thorough history of your symptoms and a physical examination. They may start with a blood test to measure your cholesterol levels and assess the extent of your risk for CAD. If your cholesterol levels are high, you may need to take medication to lower them. Your doctor may also order a blood test to look for signs of diabetes. They may also recommend an electrocardiogram (also known as an EKG or ECG) to check for signs of a heart attack or an abnormal heart rhythm. If your doctor suspects that you have CAD, they may recommend a coronary artery calcium test. This test uses X-rays to scan your arteries and look for signs of plaque. If you have a high amount of plaque in your arteries, it could mean that you have CAD.
Treatment of coronary artery disease
If you have established CAD, your doctor will work with you to develop a treatment plan. Depending on your specific case, they may recommend lifestyle changes, nutrition support, medication, or even surgery. In certain cases, doctors may even recommend a procedure called a percutaneous coronary intervention (PCI). This minimally invasive procedure can help you reduce your risk of heart attack by removing plaque from your coronary arteries. The treatment options include interventional procedures and treatments with stents, coronary artery bypass grafts (CABG) or medications depending upon the case. Stents are small mesh tubes that are inserted into the arteries. Medications can help lower your cholesterol levels, blood pressure, and blood sugar. CABG is a surgical procedure that reroutes blood flow around blocked arteries.
Prevention of coronary artery disease
The best way to prevent CAD is to initiate self-care and maintain a healthy lifestyle. This means eating a balanced diet, getting enough exercise, and maintaining a healthy weight. A healthy diet and an active exercise routine will help you in your journey to maintain a healthy weight and improve your heart health. A healthy diet should consist of various fruits, vegetables, lean proteins, whole grains, low-fat dairy products, and salt-free table salt.
Make sure to maintain healthy blood pressure and cholesterol level and a moderate body mass index (BMI, a measurement of body fat based on height and weight). These will help prevent CAD and reduce your chances of a heart attack or stroke. The best way to prevent CAD is by managing your risk factors. This means taking steps to reduce your risk of developing each of the risk factors for CAD. With the right lifestyle changes, you can greatly reduce your risk of CAD and heart disease. Some of the most important lifestyle changes include eating a healthy diet, getting regular exercise, and managing your stress levels. Your doctor would prescribe certain medications for controlling cholesterol, reducing chances of blood clots formation, and maintaining healthy blood pressure, if need be. If you’re concerned about your risk of developing CAD, it’s important to visit your doctor and have them perform a full checkup. During your appointment, they’ll ask you about your medical history, lifestyle, and family history. They’ll also perform a physical exam and order any necessary tests to help you get a better understanding of your current heart health. Based on the results of your tests, your doctor may recommend lifestyle changes, medication, or even surgery to reduce your risk of CAD.
Tips for improving coronary artery health
If you’re concerned about your risk of developing CAD, there are several things you can do to protect your heart. Make sure you’re getting enough exercise. The best exercise is one that you enjoy and that you can do regularly. It’s also important to make sure you’re getting enough sleep, managing your stress levels, and following a healthy diet. To help prevent CAD and improve your heart health, follow these tips:
- Stay away from tobacco products.
- Maintain a healthy weight, and eat a balanced diet that’s rich in fruits and vegetables.
- Get your cholesterol and blood pressure checked regularly.
- Keep your diabetes under control with regular exercise and a healthy diet.
- Visit your doctor regularly and get your blood pressure checked.
Conclusion
Knowing the symptoms, risk factors, and treatments for CAD can help you protect yourself and those around you from its potentially devastating effects. In this article, we’ve explored what you need to know about coronary artery disease and how to identify and manage it. We’ve also discussed aspects of treatment options and preventive measures. If you have any of the above-mentioned CAD risk factors, it is essential to be evaluated for CAD, even if you do not experience symptoms. Following a healthy diet and exercise routine is essential to maintain a healthy heart.
FAQs
At what age do your arteries start clogging?
Research has shown that on an average the from the age of 35 and upwards, most men and women start to have blocked arteries.
What are the signs that your heart is weak?
Signs like shortness of breath on exertion, chest pain, fatigue, and swelling of the legs, ankles, and feet indicate the heart is weak.
What does a blocked artery feel like?
A blocked artery will induce symptoms of chest pain and tightness, and shortness of breath.
Can an ECG detect a blocked artery?
An ECG can detect a blocked artery. Also, your cardiologist may recommend an ultrasound to check for blockages
Is coronary artery disease and heart disease same?
Cardiovascular disease or heart disease refers to a cluster of diseases related to the heart, including coronary heart disease.
Does coronary artery disease require surgery?
If the arteries are blocked in several areas, or if there is a blockage in one of the larger main arteries, then coronary bypass surgery will be recommended.
Can a blocked artery clear itself?
No, a blocked artery does not clear itself.
What is the test recommended for coronary artery disease?
Coronary Angiography, also called cardiac catheterization, is the recommended test for diagnosing coronary artery disease.