Coronary Artery Disease (CAD) is the number one cause of death, disability, and human suffering globally. Once you are diagnosed with CAD you have to learn to live with it by adopting a lifestyle that fits you and your heart health. By lowering the risk factors, you can live your life despite having CAD.
There is a possibility that you may be living with CAD long before you realize it. It creates fear and anxiety due to the close association with heart attacks.
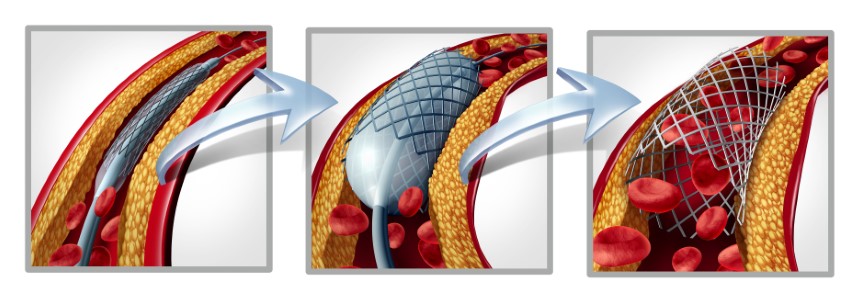
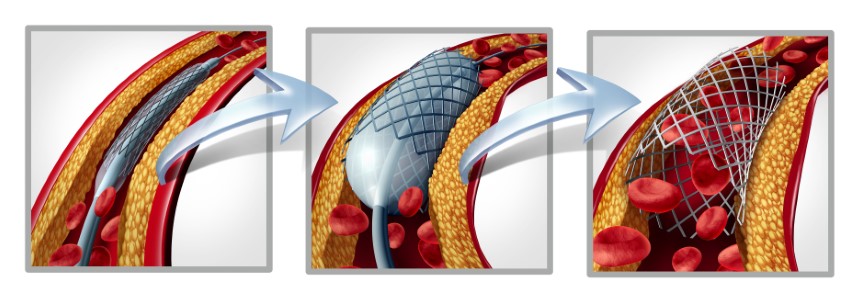
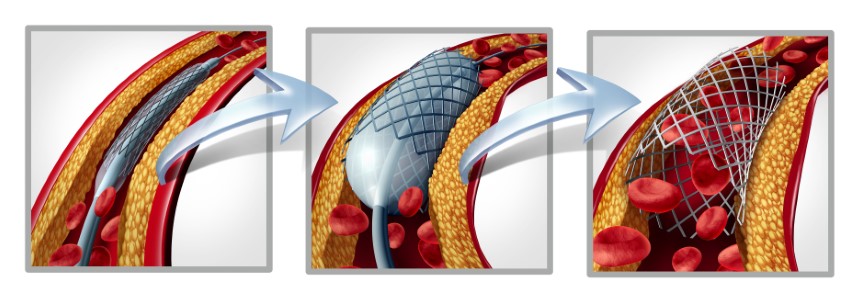
Coronary artery disease occurs when your heart’s primary blood arteries become damaged or diseased. Coronary artery disease is caused by cholesterol-containing deposits (plaques) in your coronary arteries and inflammation. The coronary arteries supply your heart with blood, oxygen, and nourishment. Plaque development can restrict these arteries, reducing blood flow to the heart. Reduced blood flow may eventually result in chest pain (angina), shortness of breath, or other signs and symptoms of coronary artery disease. A heart attack might be caused by a total blockage. Although Coronary Artery Disease (CAD) is not completely curable, the doctor would suggest an option of a procedure known as Percutaneous Coronary Intervention (PCI), which allows one to live a normal life. Coronary angioplasty, also known as percutaneous coronary intervention, is a non-surgical procedure for treating obstructive coronary artery disease that involves inserting a stent through a catheter (a thin flexible tube) into the blocked arteries.
Why is it done?
Coronary Angioplasty restores blood flow to the heart muscle and can improve symptoms of blocked arteries, such as chest pain and shortness of breath.
Does stenting improve long-term survival?
Not guaranteed. It saves your coronary, but stents do not increase a cardiac patient’s long-term survival rate. However, they do give a considerable early and sustained reduction in the requirement for subsequent treatments to reopen the treated artery. While studies have indicated that placing stents in newly re-opened coronary arteries reduces the need for repeat angioplasty procedures, it has also shown that stents do not affect death overtime. The findings have significant economic and clinical consequences for doctors considering whether to perform coronary artery bypass surgery or less-invasive angioplasty with stent implantation on their heart patients.5 According to medical opinion, your stents can help you live longer if you manage your other risk factors as per your cardiologist’s recommendations. Diet and exercise, however, are the most important factors to consider. Your risk factors for a heart attack, such as hypertension, diabetes, and obesity, can be controlled by the type and amount of food you eat. Along with these two critical components, follow your cardiologist’s advice and take your prescribed medicines on time to manage your blood pressure, diabetes, and cholesterol. As a result, even after implanting stents in three major coronary arteries, if correctly controlled, you can live a long life.
If you have a heart attack in your late thirties and have stents, is it likely you will not have an average life expectancy?
Over the last few decades, aging has been identified as one of the leading causes of heart attacks, affecting men and women aged 50 and up. People in their 20s, 30s and 40s are now more likely to suffer from cardiovascular attacks.
The guidelines emphasize lifestyle changes and the proper use of medicines as first-line treatment in adults with stable CAD. However, for people suffering from Non-ST Segment Elevation Myocardial Infarction aka NSTEMI (substernal pain while resting or with minimal exertion) and unstable angina; clinical insight is required to assess if other procedures such as CABG (Coronary artery bypass graft) or OMT (Optimal medical therapy) are more appropriate.
Whatsoever the application, PCI should not be viewed as a ‘fast cure’ but rather as a procedure that should be discussed with your doctor to balance the benefits, risks, and limitations.
Source:
- https://www.narayanahealth.org/blog/coronary-artery-disease-life-expectancy-and-prognosis/
- https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
- https://www.heartandstroke.ca/heart-disease/treatments/surgery-and-other-procedures/percutaneous-coronary-intervention
- https://www.onhealth.com/content/1/stents_save_coronaries_not_lives
- https://www.verywellhealth.com/do-angioplasty-and-stents-prolong-life-4021221