In India, diabetes is a widespread health issue affecting millions. According to WHO, about 77 million adults have type 2 diabetes [1]. But did you know that diabetes affects more than just your blood sugar? Many are unaware of its link to other conditions, like peripheral vascular disease (PVD). PVD impacts blood vessels outside the heart and brain, and when combined with diabetes, it can lead to severe complications. Find out how diabetes and PVD are connected and how you can manage both conditions effectively.
What is Peripheral Vascular Disease? [2]
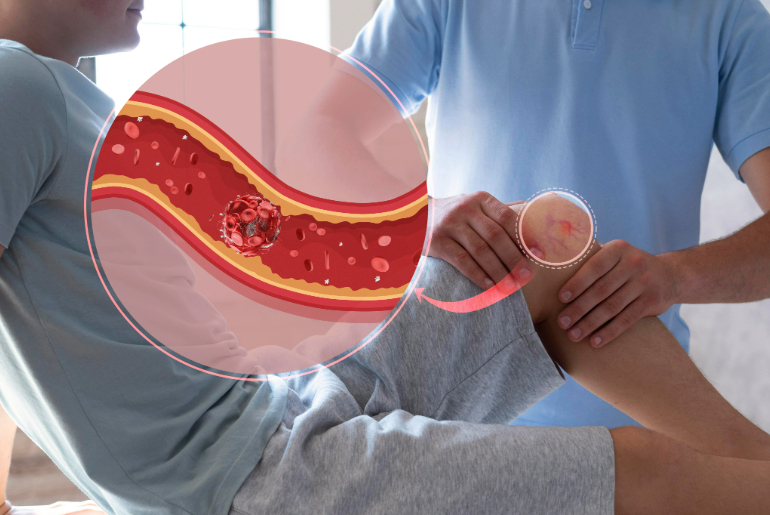
Peripheral vascular disease (PVD) affects the blood vessels, especially in the legs and feet. In PVD, arteries narrow or get blocked due to fatty deposits, reducing blood flow to the limbs. This can cause pain, cramps, and sores that take longer to heal. If not treated, PVD can lead to serious problems like infections, tissue damage, or even amputation in severe cases. PVD is more common in people with other health conditions, including diabetes.
The Connection Between Diabetes and PVD [3]
Diabetes and peripheral vascular disease (PVD) are closely connected because diabetes also affects blood vessels. High blood sugar can damage the blood vessel lining, making it easier for fatty deposits to form and block the arteries, especially in the legs and feet. This is a key feature of PVD. People with diabetes are more likely to develop PVD since their blood vessels are more vulnerable to damage. High blood sugar also slows down the body’s ability to heal wounds, increasing the risk of complications from PVD.
Both diabetes and PVD get worse over time if not properly managed. The reduced blood flow caused by PVD can make it harder for diabetes-related foot problems, like ulcers, to heal. This can lead to infections. In severe cases, surgery may be needed.
Common Symptoms Linking Diabetes and PVD [3]
People with both diabetes and peripheral vascular disease often experience similar symptoms, especially in the legs and feet. Some common signs to watch out for include:
- Leg pain or cramping – This can happen during activities like walking and is called claudication. It occurs because the muscles are not getting enough blood flow.
- Numbness or tingling in the legs or feet – This may result from nerve damage caused by both diabetes and PVD, making it harder to feel injuries or infections.
- Slow-healing sores – Wounds, especially on the feet, may take longer to heal due to poor blood flow and high blood sugar levels.
- Coldness in the lower legs or feet – This is a sign of poor circulation caused by peripheral vascular disease.
- Shiny or discoloured skin – Poor blood flow can change the appearance of the skin, especially in the lower legs and feet.
If any of these symptoms are present, it is always recommended to seek medical advice early to prevent further complications.
Risk Factors & Complications [3]
Several factors can raise the chances of developing both diabetes and peripheral vascular disease. These include:
- High blood pressure – It puts extra pressure on blood vessels, making them more likely to get damaged.
- High cholesterol – Too much cholesterol can cause fatty deposits in the arteries, leading to PVD.
- Smoking – Smoking harms blood vessels and greatly increases the risk of PVD, especially in people with diabetes.
- Obesity – Being overweight adds strain on blood vessels, raising the risk of both diabetes and PVD.
- Sedentary lifestyle – Not being physically active can lead to poor circulation, making it harder to control blood sugar levels. This also increases the risk of PVD.
If not managed properly, complications from diabetes and PVD can be serious. Poor circulation from PVD can cause infections, slow-healing wounds, and, in severe cases, gangrene, which might require amputation. Additionally, people with both conditions have a higher risk of heart attacks and strokes.
Preventive Measures for Diabetes and PVD [3]
- Blood sugar control – Keeping your blood sugar at a healthy level is crucial to avoiding complications from diabetes, including peripheral vascular disease.
- Regular exercise – Being physically active helps improve blood circulation and lowers the risk of PVD by promoting healthy blood vessels.
- Healthy diet – Eating a balanced diet that is low in saturated fats, salt, and sugar can help stop fatty deposits from building up in the arteries.
- Quit smoking – Smoking is a big risk factor for both diabetes and PVD. Quitting can greatly reduce the chances of complications.
- Foot care – For diabetics, taking care of your feet is important. Checking your feet regularly for wounds or sores and getting treatment quickly can prevent serious problems.
Conclusion
It’s clear that diabetes and peripheral vascular disease (PVD) are more connected than many realise. But here’s the good news—by staying informed and taking proactive steps, you can manage both conditions effectively. Remember, the key is catching the signs early and taking control.
Reference Links:
[1] https://www.who.int/india/health-topics/mobile-technology-for-preventing-ncds
[2] https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-vascular-disease
[3] https://www.medicalnewstoday.com/articles/diabetes-peripheral-vascular-disease#treatments