What are sinus headaches / Rhinogenic Headache?
Have you ever felt under pressure around your eyes and cheeks, and your head is throbbing? It would appear that you have another Sinus headache / Rhinogenic Headache.
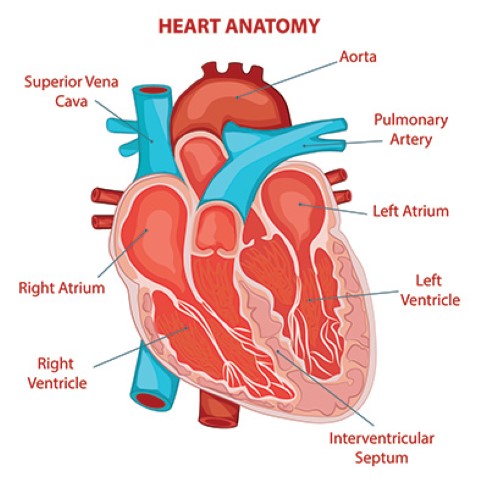
Sinusitis/rhinosinusitis is an inflammation of the tissues lining the sinuses. It leads to poor or blocked sinus drainage and causes congestion, headaches, runny nose, loss of smell and taste, and infections. Worldwide it affects millions of people every year.
Acute vs. Chronic
Acute sinusitis only lasts for a short period, as stated by the American Academy of Otolaryngology. Usually, it’s less than four weeks. In an acute infection, the patient suffers from a part of a cold or other respiratory illness.
Chronic sinus infections last for more than twelve weeks or recur periodically. Allergies & nasal polyps are noticed in these patients.
Symptoms Of A Sinus Headache / Rhinogenic Headache
- Pain, pressure, and fullness in your cheeks
- Uncomfortable pressure behind the forehead
- Stuffy nose
- Runny nose
- Fatigue
- Green or yellow nasal discharge and congestion
- Achy feeling in the upper teeth
- Allergies & nasal polyps lead to sinus pain and symptoms
Causes of a Sinus Headache / Rhinogenic Headache:
Sinus headaches / Rhinogenic Headache are triggered by allergic reactions or changes in weather. Allergy caused by pollen or dust – affects the mucous membranes leads to our eyes watery and nose runny.
Bacterial infections, viral infections & fungal infections trigger a sinus headache. Viral infections last for a few days whereas bacterial infections can last for 7 days or beyond.
Allergic Fungal Sinusitis may affect our lung and respiratory issues and the patient has asthma or nasal polyps.
When to See an ENT
Usually, people often blame these symptoms on allergies or cold attack, headache or simply feeling the effect of weather change. However, it can be an indication of Sinusitis. Paying attention to these symptoms and the duration of occurring can help determine to visit an ENT specialist.
Treatment for Sinus headache / Rhinogenic Headache
Your ENT specialist may treat your sinus headache with pain relievers, allergy medications, antibiotics, decongestants, or steroids.
Indian J Otolaryngol Head Neck Surg. 2017 suggests after performing a Clinical study, that Balloon Sinuplasty should be considered as an effective alternative option for the Treatment of Sinus headache / Rhinogenic Headache.
How Balloon Sinus Surgery Works
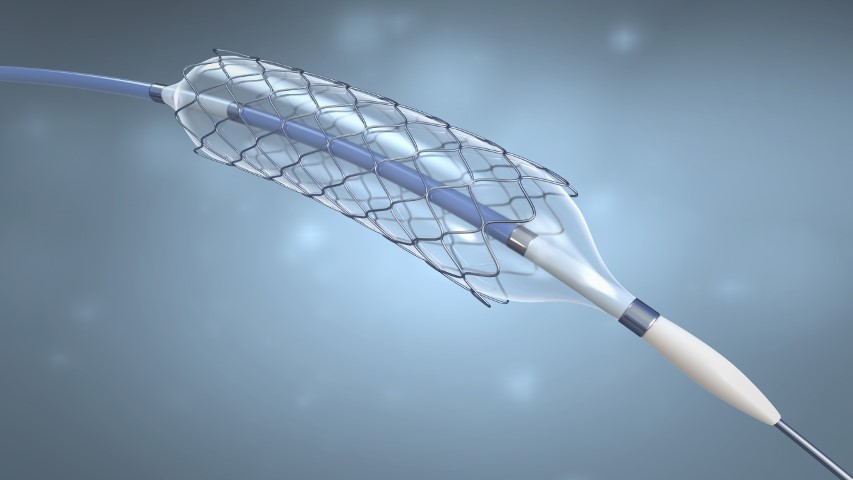
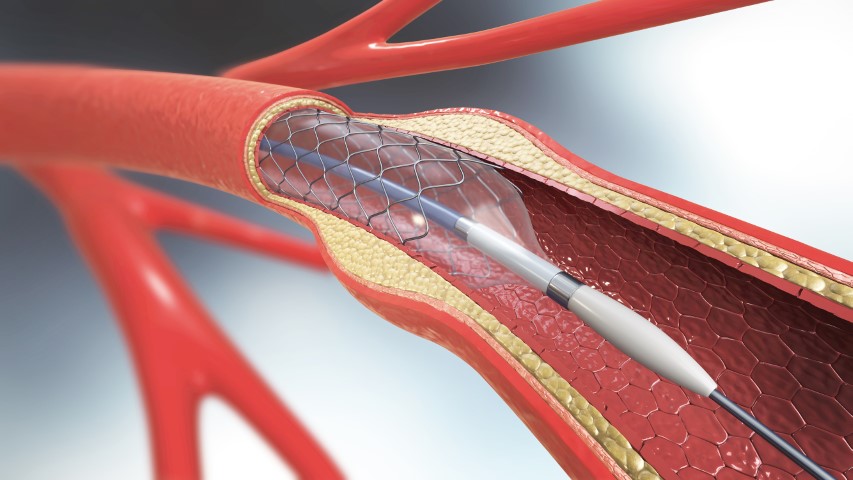
The Balloon Sinus Surgery can be performed in the ENT’s office or OT. A local or general anesthetic is applied to numb the area. Then a very small balloon catheter is inserted up through the nasal passage into the sinus. The balloon is inflated and this opens the sinus passage. The ENT flushes out the mucous and pus that has collected in the sinus with a saline solution. The balloon is removed and the sinus passage stays open.
When the balloon is inflated, it permanently alters the structure of the sinus opening. The passage not only is opened by the balloon, but it also stays open afterward. This keeps the sinus from being blocked. Because the sinus isn’t blocked it drains properly. Since the sinuses are draining you don’t get sinus headaches. It’s a cure for sinus headaches that lasts.
Balloon sinuplasty is a new technology for treating Sinus Headaches / Rhinogenic Headaches & chronic sinusitis. This is a UFDA approved technology. Affordable and inexpensive Balloon Sinuplasty procedures are available at several medical tourist destinations abroad. India, the USA, Mexico, Costa Rica, Jordan, and Turkey are using Balloon sinuplasty
Benefits of a balloon sinuplasty
A Balloon sinuplasty can treat Sinus Headache, chronic sinusitis, opening your blocked sinuses & you will get relief. This is perhaps the biggest benefit of a balloon sinuplasty. Here are some more benefits.
1. This is a minimally invasive procedure
The balloon sinuplasty doesn’t need an incision. The balloon is inflated and this opens the sinus passage, the cavity is cleaned and drained. No incisions or stitches!
2. The procedure takes very little time
The balloon sinuplasty can be performed in the ENT’s office or OT, and it takes about an hour.
3. Faster Recovery
Minimally invasive procedures provide faster recovery compared to traditional surgery ― and balloon sinuplasty is no exception. The majority of patients return to their normal activities within a couple of days.
4. No nasal packing
Some nasal surgeries require nasal packing to absorb any bleeding. Remember, there’s no need for incisions or bone/tissue removal with a balloon sinuplasty, so you will not experience the same post-surgical discomfort.
5. Long-lasting relief
The most rewarding benefits of a balloon sinuplasty are that the relief is Long-lasting. In a research article published in the journal Otolaryngology-Head and Neck Surgery, patients report relief for up to two years after the procedure.
Talk To The ENT About Your Sinus Headaches / Rhinogenic Headaches
If you have recurrent sinus headaches, it’s time to talk to the ENT. Make an appointment to discuss and find out if
Balloon Sinus Surgery is the best option for you. You have nothing to lose but the pain and discomfort of sinus headaches.