Piles are very common but not something you’ll want to talk to your friends or loved ones about. Many people are ashamed of having enlarged piles. They don’t like to discuss symptoms and might be reluctant to go to the doctor. Some might be afraid of having a physical examination or finding out that they have a serious illness. But seeing a doctor about your symptoms is important if you want to have the right treatment.



Today, open access to biomedical information on the internet or social media has created new opportunities for doctors and patients, but much of the information is subject to manipulation because the ordinary conventions of context and the reliability of provenance are constantly in question. Alike other medical information, Piles too have much content online. But the question is “Is it reliable?” To uncloud this confusion, on #WorldPilesDay we invited the renowned Proctologist and Lap. Colorectal Surgeon, Dr. Pravin Gore, with 21 years of experience to share his knowledge about piles and their treatment. Dr. Pravin Gore is currently practicing in Mumbai and is associated with eminent hospitals like Apollo spectra, Bhatia, Wockhardt etc. He has vast experience in laparoscopic surgeries related to problems in the colon, rectum, anus and other parts of the lower abdomen.
During his LIVE session with us on our Facebook page, Dr. Pravin Gore shared information on the following topics;
What is Piles?
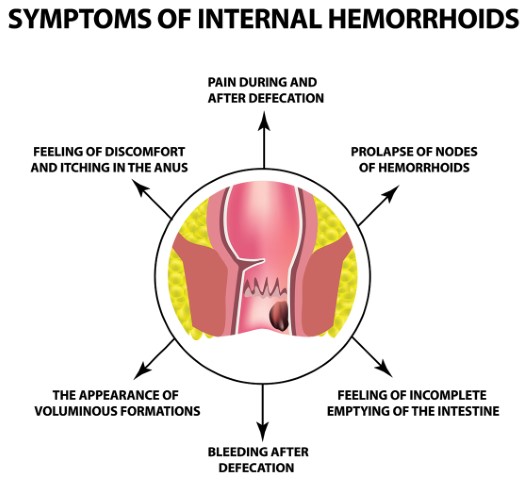
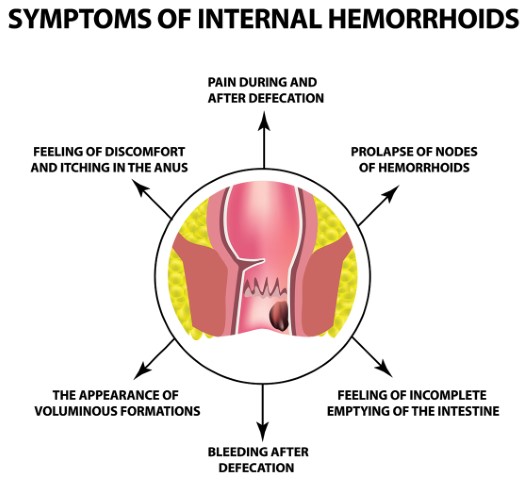
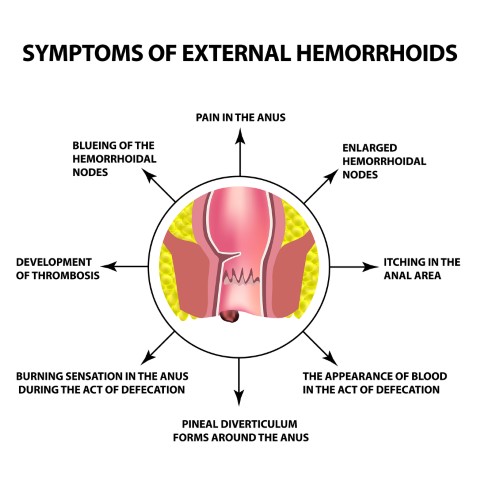
Piles, also known as haemorrhoids are swollen and inflamed veins in the rectum and anus (canal through which we pass stools) that cause discomfort and bleeding. The size of piles can vary from person to person, and they are found inside (Internal Piles) or outside (External Piles) the anus. Usually, internal piles are in the range of 2 cm – 4 cm above the opening of the anus, whereas external piles appear on the outside boundaries of the anus.
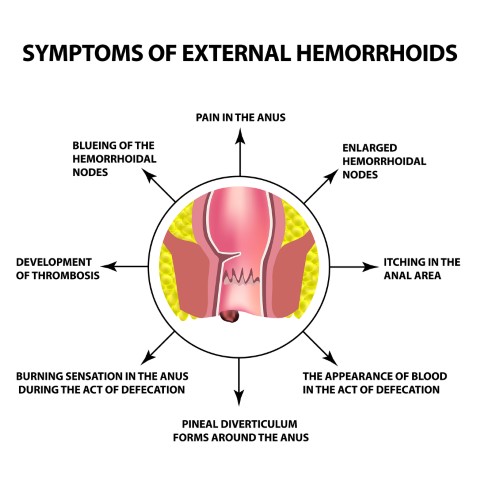
Symptoms and Causes of Piles
In most cases, the symptoms of piles are not serious. One of the most common symptoms of piles is bleeding post passing stools. Sometime you will notice no symptoms or signs at all. Nonetheless, a piles patient may experience:
- A hard and painful mass which is present around the anus.
- Feeling of bowels being full, even after passing of stools.
- Noticing bright red blood after passing stools, on the toilet paper or toilet pan.
- Itching and inflammation of the anal area.
- Pain while passing stools.
Usually, piles are caused by increased pressure in the lower rectum. Also, sometimes piles tend to develop for no apparent cause but there are specific circumstances that may certainly increase the chances of one developing piles such as:
- Chronic constipation
- Chronic diarrhoea
- Lifting heavyweights
- Pregnancy
- Straining when passing a stool
- Cancer in the colon
How to prevent piles?
Fortunately, there are numerous precautions to prevent piles from interfering with your daily life.
- Fibre-rich diet
- Drink plenty of water
- Regular exercise
- Avoid frequent use of laxatives
- Don’t hold your bowel movements
- Avoid straining
How much time does it take to cure piles?
Usually, small piles may clear up without any treatment within a few days (7-10 days) and you will be able to resume most activities right away. However, large or external piles may take longer to heal depending upon the treatment.
What are the treatment options available for Piles?
If detected at an early stage, piles can be treated with just medication and lifestyle changes such as consumption of high-fibre diet to prevent constipation, taking OTC (Over-the-counter) medicines such as creams (Hydrocortisone – a medication used to treat swelling, redness and itching), painkillers, etc.
If there’s no improvement to your piles after home treatments and medications, you may require other minimally invasive procedure such as:
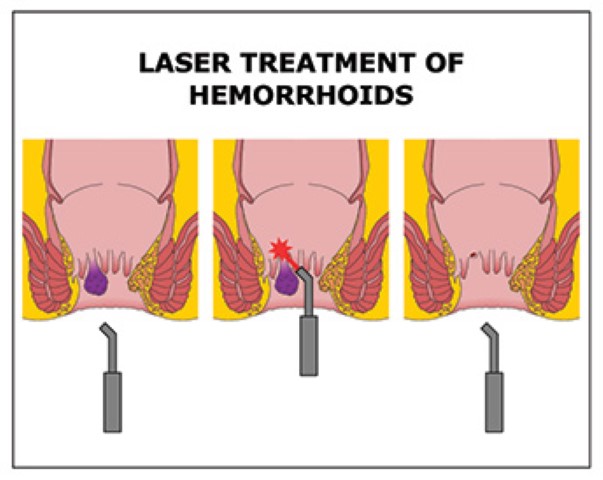
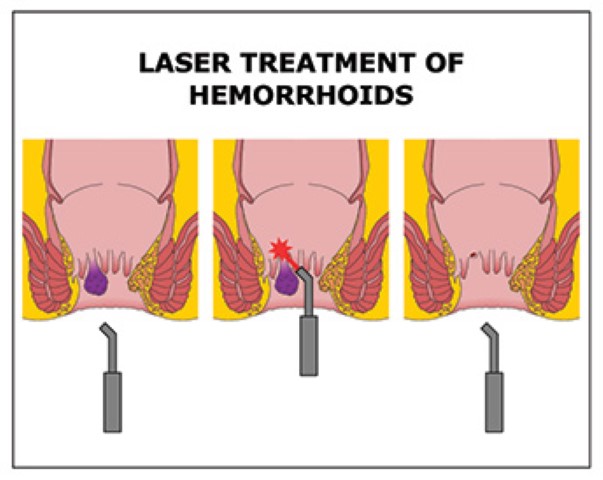
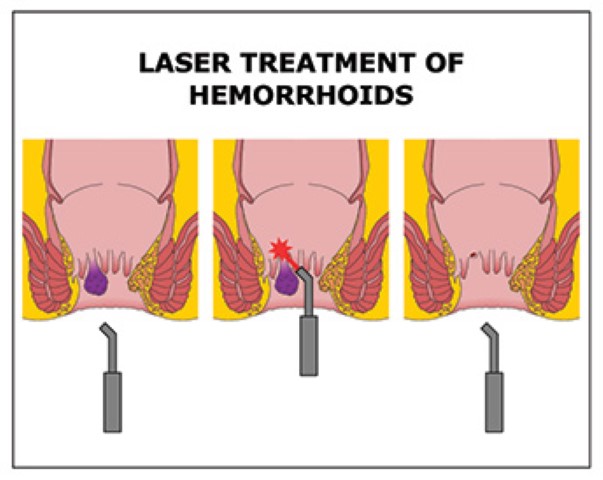
- Coagulation (infrared or laser): This treatment is for internal piles. The technique uses infrared light or laser to harden and shrivel the internal piles.
Other surgical treatment options include:
- Haemorrhoidectomy: Haemorrhoidectomy refers to the surgical removal of internal or external piles. This procedure is considered to be the most effective way to treat severe or recurring piles.
In this method, piles are diagnosed and removed using a sharp instrument or laser and the wounds are then closed by stitching.
- Stapling: This method is an alternative to haemorrhoidectomy and is also used for prolapsed piles. The procedure includes stapling the last section, anal canal of the large intestine, which reduces blood supply to the piles and causes them to slowly shrink. It also lowers the likelihood of haemorrhoids prolapsing. According to Dr. Pravin Gore, Meril’s MIRUS Hemorrhoids Stapler offers better security and superior haemostasis which delivers optimum excision of prolapsed haemorrhoidal tissue. Stapling generally involves less pain than the other procedure and allows an earlier return to your regular activities.
- Other treatment options include band litigation, Haemorrhoid artery litigation & Sclerotherapy.
What are the chances of Piles relapsing after the surgery?
There are no chances of piles relapsing after the surgery if the piles are removed from the anal canal, but when the piles are just sealed with other treatment options, then there are 10% chances of relapsing. However, the reoccurrence of piles can also be well managed by avoiding constipation and straining while having bowel movements.
What is the difference between piles, fissures, and fistula?
Piles are mainly the swollen blood vessels in the anal canal, which occurs due to chronic constipation while fissures are kind of the cracks found in the skin of the anal canal and fistulas are the small opening in the anal canal, it is kind of cavity filled with pus.
Opting for the right treatment option completely depends on the severity of the condition and should be considered after consulting with your doctor. Summing up, if anyone is suffering from piles or has bleeding or pain from their anal canal should visit their doctor immediately. Because delay in the treatment can make the condition worse.