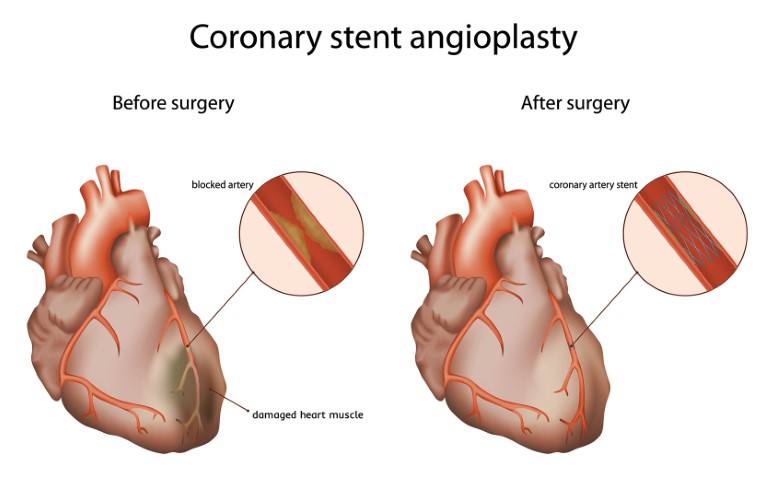
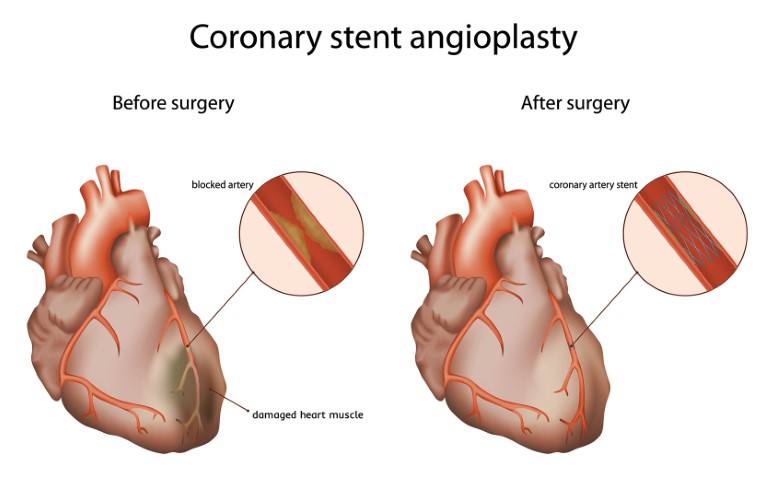
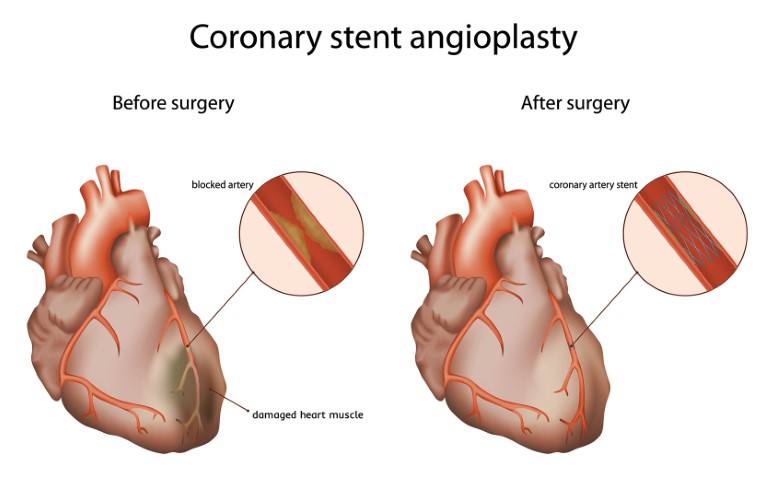
Coronary angioplasty also called stenting is the process to open or widen a blocked or narrowed coronary (heart) artery that occurs due to heart disease. This blockage happens because of the build-up of a waxy substance called plaque. Angioplasty surgery restores and enhances the normal blood flow in the affected arteries. Thus, rich oxygenated blood reaches your heart reducing the risk of stroke or heart disease and promoting quality improvement in life. Angioplasty is also often used during a heart attack to open a narrowed artery and reduce the amount of damage to your heart.
Angioplasty vs Bypass surgery
Angioplasty and bypass surgery are medical procedures that are used to treat clogged, blocked or narrowed arteries in the heart.
Bypass surgery is a major procedure that involves taking a healthy blood vessel from your leg, arm or chest and connecting it below and above the blocked arteries in your heart. With a new pathway, blood flow to the heart muscle improves. This takes much longer surgery as well as recovery time as compared to angioplasty. It usually involves doctors cutting the chest to get to the heart to conduct the surgery. The patient needs a longer hospital stay and around two weeks of recovery time.
On the other hand, angioplasty does not require major surgery, it usually requires a small incision in the leg, arm, or wrist and gets completed in an hour approximately. The procedure is less invasive and has a relatively rapid recovery process. As a result, angioplasty or stenting is preferred to be a better procedure over heart bypass surgery.
Undergoing a coronary angioplasty might be stressful. But who said life won’t be the same after the surgery? You can enjoy a quality-life after an angioplasty or heart bypass surgery. It usually takes a couple of weeks to start returning to normal life after the surgery. Angioplasty procedure improves the way of living in several ways.
- Energized body
In coronary angioplasty, the blocked arteries in your heart are widened resulting in the restoration of the normal flow of oxygenated blood to your lungs. This also decreases the chances of heart diseases, stroke, or heart attack. The symptoms related to heart diseases like chest pain or troubled breathing also decrease. As a result, your body has more energy to carry out daily activities.
- Flourishing Lifestyle
After an angioplasty procedure, people are advised to resort to a healthy diet, to stop habits like smoking or drinking, and to exercise more often. These changes in the lifestyle help in living a quality life after any heart surgery.



- Stress-free life
Anger, anxiety, hypertension, and depression are all linked to heart disease. After having surgery, you will eventually be able to control these emotions. This will result in a sense of inner peace and a less stressful life, which in turn will keep your heart and blood vessels healthy.
- Healthy diet
After angioplasty/stenting, it is of utmost importance to follow a healthy diet regime to live a disease-free life ahead. This will push your body to heal faster and reduce risk complications. Doctors advise a diet rich in fruits, vegetables, whole grains, nuts, and seeds to reduce your risk of heart disease and enhance your life.
- Exercise to Energize
Exercising is considered to be one of the important practices on the path of living a healthy and improved life after coronary angioplasty. It helps to control the blood pressure, cholesterol levels, weight, fitness level and keeps you relaxed. And this is exactly what your body needs to retain a healthy living.



- Take Medications on time
It is important to take the medicines prescribed by your doctor on time. They help to prevent the tiny clots from forming in your stent. Go to timely check-ups and examine your risk factors and problem areas. If you have any pre-existing conditions like diabetes or high blood pressure, make sure they are under control. Once you are through with your post-surgery condition, you know to take care of yourself. A quality life awaits you after the surgery.
- Keep a tab on your weight
Maintaining a healthy weight is necessary after coronary angioplasty to improve blood pressure, blood sugar levels, and cholesterol. If you are overweight, ask your doctor or health-care provider to set up a weight-control program.



- Get ample sleep
Lack of sleep can result in the worsening of your situation even after surgery. Try sticking to a regular bedtime, every night and avoid alcohol or caffeine that may harm your sleeping schedule.
- Significant health improvements
After successful coronary angioplasty, the body starts showing significant improvements in cardiac symptoms (decreased pain in the chest), increased tolerance (able to walk an extra mile without any trouble), better physical functioning and vitality. In case, you are still experiencing symptoms similar to those you had before the surgery, like chest pain or breathlessness, contact your doctor. Heath improves for better after the surgery to avoid complications like a heart attack or stroke in the future.
- Maintain a positive perspective
Coronary angioplasty is a crucial emergency step or a planned procedure taken to prevent further life-threatening heart conditions. Undergoing an angioplasty procedure can be quite scary, but it’s necessary to accept the situation pragmatically to live a healthy life in the future. A positive outlook reinforces high-quality life.
Going through coronary angioplasty is an emotional rollercoaster. It substantially improves the perceived quality of life of the patient as compared to being dependent on medicines. Undergoing an angioplasty or stenting doesn’t mean your heart disease goes away. You’ll need to continue following healthy lifestyle habits and take medications as prescribed by your doctor. After the surgery, before you leave the hospital, you will be briefed about detailed instructions for the exercise, follow-up appointments, post-surgery care, medications, and resuming daily activities. It is necessary to follow these guidelines thoroughly to heal faster and enjoy a safer and quality life.