Have you ever felt a strange pain in your legs while walking that eases up when you rest? This could be a sign of something more than just tired muscles. Peripheral artery disease (PAD) is a condition that many people have but are unaware of. This article explores the basics of peripheral artery disease, its risk factors, potential complications, and simple steps you can take to protect your arteries.
What is Peripheral artery disease?[1]
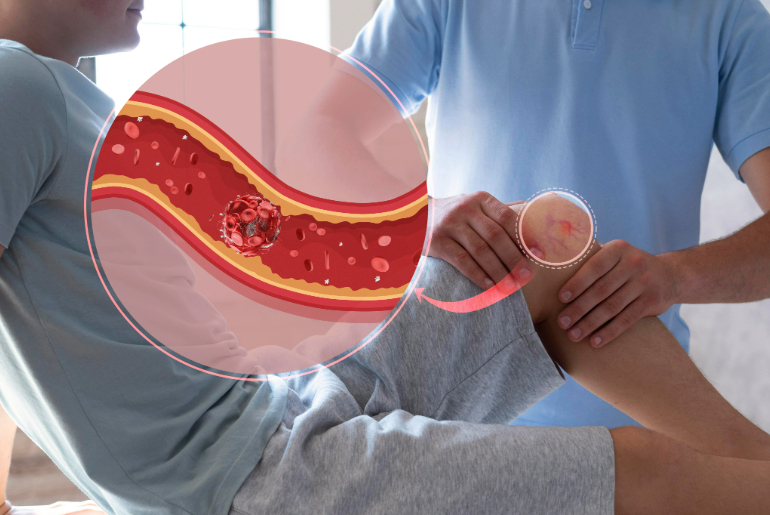
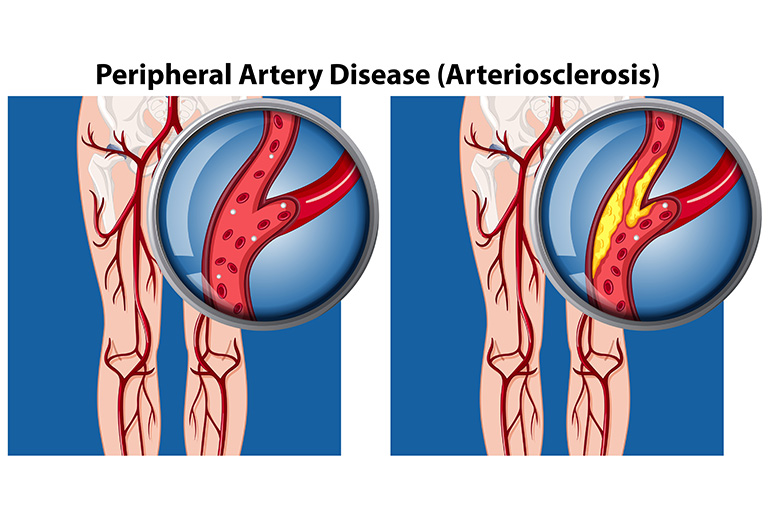
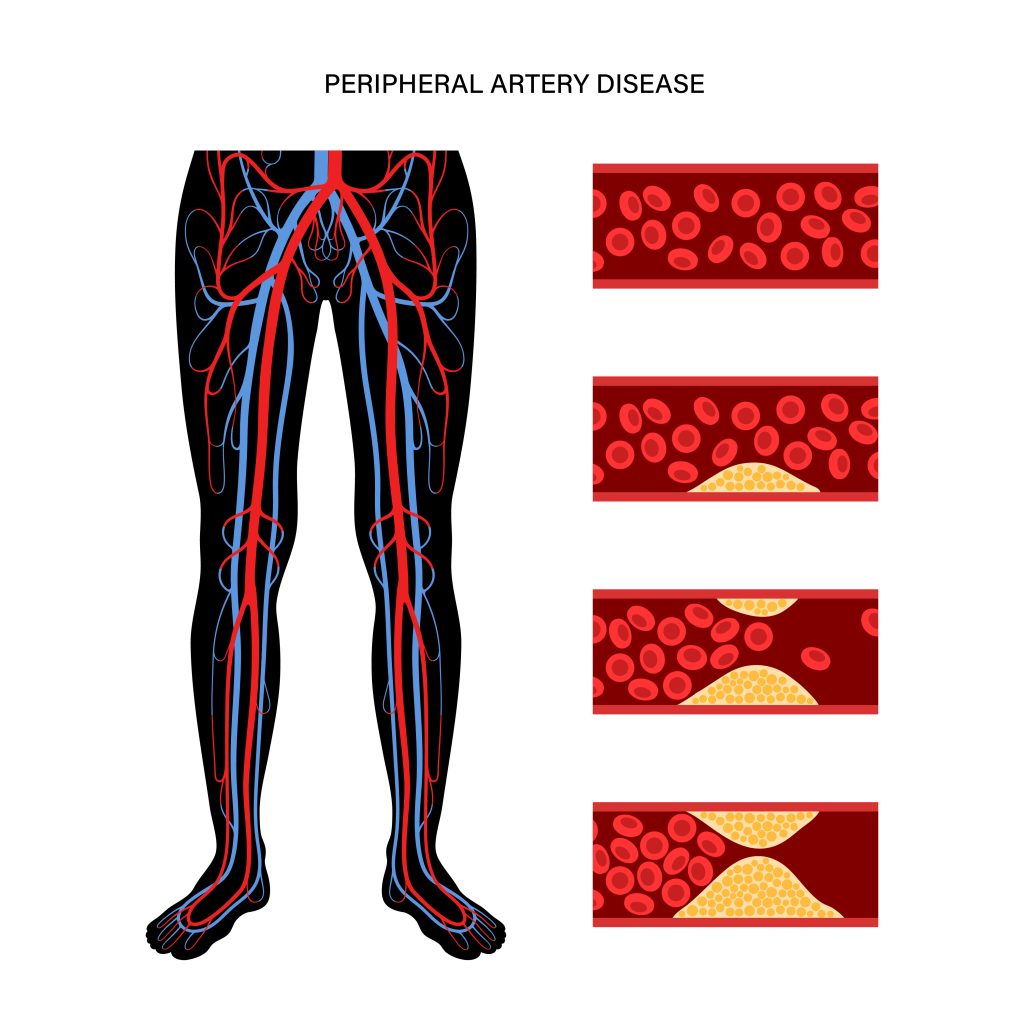
This is a condition where the arteries, which supply blood to the limbs, become narrowed or blocked. This happens due to a build-up of fatty deposits called plaque. When these arteries are narrowed, blood flow to the legs and other extremities is reduced, causing pain and other symptoms. The legs are the most commonly affected areas, leading to pain while walking, known as claudication.
Risk Factors for Peripheral artery disease[1]
a. Lifestyle Factors
- Smoking: The chemicals in tobacco have the potential to damage the blood vessels. This makes it easier for plaque to build up and narrow the arteries.
- Diet: A poor diet that is high in saturated fats, trans fats, and bad cholesterol can be one of the reasons behind the build-up of plaque in the arteries. Eating a healthy, balanced diet with plenty of fruits, vegetables, and whole grains might help to reduce the risk.
- Physical Inactivity: Regular physical activity helps to maintain healthy blood flow and keeps the arteries well, helping them function and keeping disease at bay.
b. Health Conditions
- Diabetes: High blood sugar levels might damage the blood vessels and contribute to plaque build-up.
- Hypertension: High blood pressure puts extra strain on the arteries, which can lead to the damage and narrowing of these blood vessels.
- High Cholesterol: Plaque formation can also occur due to elevated levels of cholesterol in the blood, increasing the risk of peripheral artery disease.
c. Demographic Factors[2]
- Age: Older adults are more likely to develop this condition due to the natural hardening of the arteries over time.
- Gender: Men are usually at a higher risk of developing peripheral artery disease than women. However, postmenopausal women also face a significant risk.
- Family History: A family history of peripheral artery disease or other cardiovascular diseases can increase the likelihood of developing this condition.
Complications of Peripheral artery disease[2]
- Critical Limb Ischemia: This is a severe condition where the blood flow to the limbs is significantly reduced, causing severe pain and potentially leading to sores or ulcers that takes time to heal.
- Stroke and Heart Attack: There is an increased risk of stroke and heart attack as this condition affects the arteries supplying blood to the heart and brain.
- Infections: Reduced blood flow can impair the healing of wounds and inadvertently increase the risk of infections.
- Amputation: In severe cases, the lack of blood flow might lead to tissue death and the need for amputation of the affected limb.
Prevention of Peripheral artery disease[2]
a. Lifestyle Modifications
- Quitting Smoking: Stopping smoking can significantly improve vascular health and reduce the risk of peripheral artery disease.
- Healthy Diet: Eating a healthy, well-balanced diet like fruits, vegetables, and whole grains is necessary as it helps maintain healthy arteries and reduces the risk of plaque build-up.
- Regular Exercise: Regular physical activity, such as walking, cycling, or swimming, improves circulation and overall vascular health.
b. Managing Health Conditions
- Diabetes Management: Blood sugar levels should be kept under control to reduce the risk of peripheral artery disease in people with diabetes.
- Blood Pressure Control: Maintaining healthy blood pressure through lifestyle modifications and, if necessary, medication helps protect the arteries from damage.
- Cholesterol Management: Keeping cholesterol levels in check through diet, exercise, and medication can prevent plaque build-up in the arteries.
c. Regular Check-ups
- Importance of Routine Health Screenings: Regular check-ups with a healthcare provider can help detect peripheral artery disease early and manage any risk factors effectively.
- Discussing Symptoms Early: Reporting any symptoms, such as leg pain or numbness, to a healthcare professional can lead to early diagnosis and treatment.
Conclusion
Peripheral artery disease might sound intimidating, but understanding it is the first step towards taking control of your health. Don’t wait for symptoms to appear—start making healthier choices today. If you have any concerns, make sure to consult a healthcare professional and get regular check-ups.
Reference Links:
[1] https://www.heart.org/en/health-topics/peripheral-artery-disease/about-peripheral-artery-disease-pad#:~:text=Peripheral%20artery%20disease%20is%20similar,to%20the%20legs%20and%20feet.
[2] https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-vascular-disease