Introduction
Thrombosis comes from the Ancient Greek – thrómbōsis, which means ‘clotting.’ It is the process of the formation of a blood clot inside a blood vessel and is also known as a thrombus. In the process, it causes blocking and obstructs blood flow in the affected area resulting in complications, especially if the clot moves to a critical part of the circulatory system, the brain, or the lungs.
In the event of an injury of a blood vessel, either a vein or an artery, it is very typical for the human body to prevent further blood loss by using thrombocytes or platelets and fibrin to form a blood clot. When a piece of the blood clot or the clot breaks free, it can form an embolus that moves around the body in the bloodstream, obstructing blood flow to critical organs like the brain or the lungs, resulting in reduced oxygen supply and blood flow with severe complications.
Types of Thrombosis
Now that you know thrombosis occurs when blood clots block blood vessels, you will discover that there are two broad classifications of thrombosis depending on the type of blood vessel affected (arterial or venous) and the exact location of the blood vessel or the organ supplied by it.
Venous Thrombosis – When thrombosis occurs in the veins or the blood clot blocks a vein, it is called venous thrombosis, also known as DVT, which stands for deep vein thrombosis. In this case, there is a blood clot in the affected part of the body, like the deep veins, axillary or subclavian veins (deep veins of the upper limb), hepatic veins (veins that drain venous blood from the liver), renal vein (the major blood vessel carrying blood from the kidney and the ureter), or jugular veins (veins located within the carotid sheath on either side of the neck). Veins typically from different parts of body to the heart.
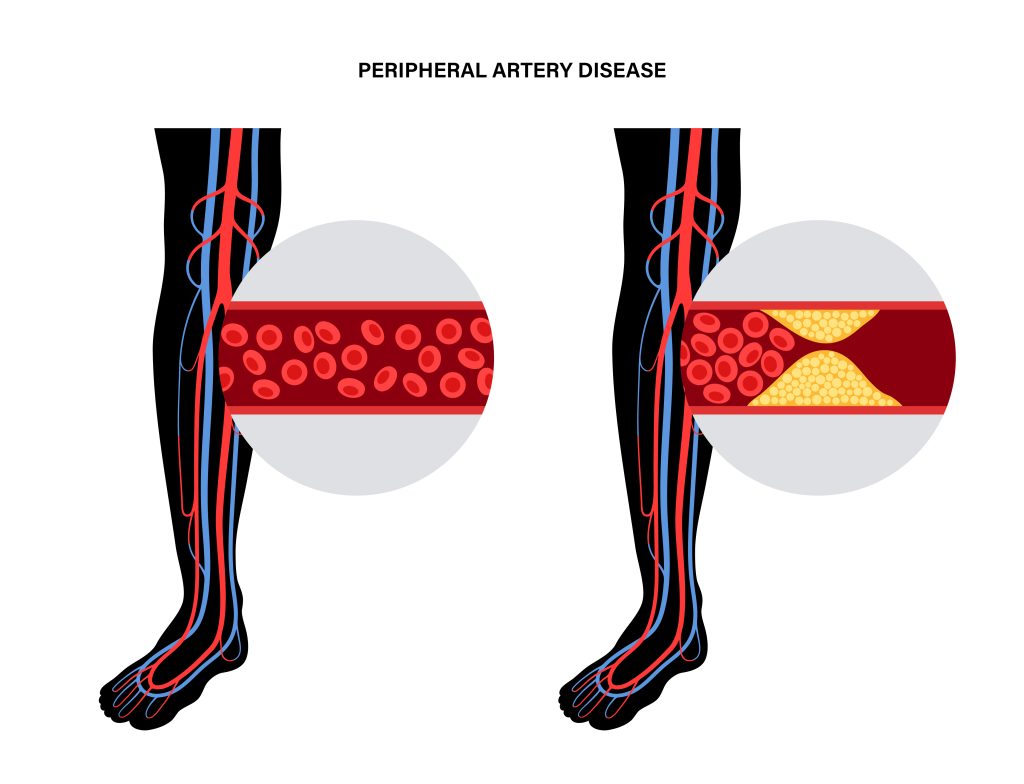
Arterial thrombosis – When thrombosis occurs in the arteries, and the blood clot blocks an artery, it is known as arterial thrombosis. Arteries carry oxy-rich blood from the heart to the rest of the body. In the case of arterial thrombosis, the blood supply can be affected and restricted, which can further damage the tissue supplied by that particular artery.
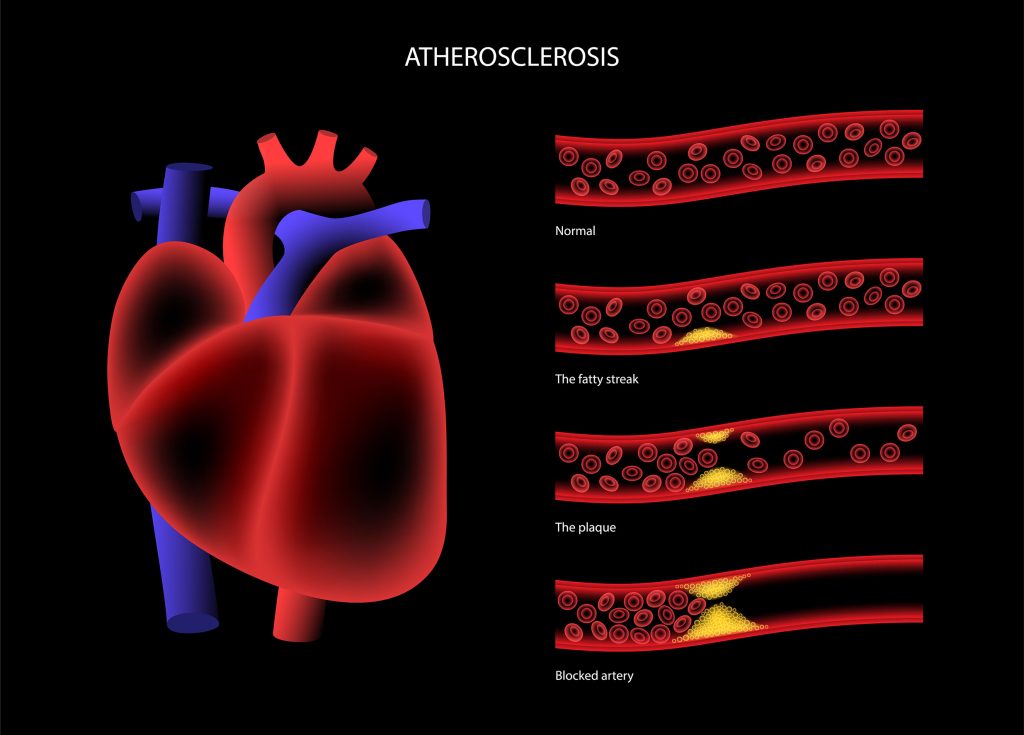
For example, if arterial thrombosis occurs in a blood vessel in the brain, or what we call arterial embolism, it can lead to a stroke. Similarly, the blood clots could migrate downstream and pose a risk affecting any organ. And if arterial thrombosis occurs in the arteries that supply blood to the heart muscle (coronary arteries), it can lead to a heart attack. The blood clots happen due to the hardening of the arteries or thickening of the artery walls, a condition called atherosclerosis in which there is a buildup of plaque or fatty deposits. This plaque buildup can lead to a rupture followed by a blood clot. Thrombus in the coronary artery can also cause myocardial infarction leading to ischemia. The reduced oxygen supply to the heart cells can often lead to cell death or necrosis.
Causes of Thrombosis
- Venous thrombosis can be caused by-
– Immobility
– Any injury or disease to the leg veins
– A fracture
– Being overweight or obese
– Certain medications that can increase the risk of clotting
– Genetic disorders
– Autoimmune disorders.
- Arterial Thrombosis, on the other hand, is caused by the hardening of the arteries, called arteriosclerosis. This typically occurs when fatty or calcium deposits make the artery walls thick, leading to a fatty buildup of plaque which can burst to cause a rupture, followed by a blood clot.
Generally speaking, some people are predisposed to developing thrombosis and thromboembolism (like newborn babies in the neonatal phase). At the same time, some have a higher risk of developing either venous thrombosis or arterial thrombosis. Also, the chances of development of this condition of thrombosis increase with age and depend on several risk factors and lifestyle factors like the ones discussed above and the following,
● Heart Condition
● Lung Condition
● Crohn’s Disease (an inflammatory bowel disease affecting the lining of the digestive tract)
● Major Fractures, burns, or injuries to the deep veins in the legs, arms, or the pelvis area
● Lack of movement and physical activity due to travel without moving, medical procedures like surgery or hospitalization, or leg paralysis
● Certain medications like birth control medicines and hormonal contraceptives which contain estrogen or chemotherapy drugs
● Any autoimmune or inflammatory disorder that promotes easy blood coagulation and blood thickening
● Any inherited gene conditions like a family history of blood clots, stroke, or heart attack
● Diet
FAQs:
What is a major cause of thrombosis?
The major cause of thrombosis could be any of the following,
– immobility
– any injury or disease to the leg veins
– a fracture
– being overweight or obese
– certain medications that can increase the risk of clotting
– Genetic disorders
– Autoimmune disorders.
What are the three factors that lead to thrombosis?
Any of the following can be risk factors for thrombosis,
– high blood pressure
– high cholesterol
– diabetes.
What is the most common thrombosis?
The most common thrombosis is arterial thrombosis, which happens in arteries that carry blood from the heart to the rest of the body, often considered to be one of the key reasons for heart attacks and strokes.
What are the signs of thrombosis?
The visible signs and symptoms of thrombosis are pain, swelling, and tenderness in one of the legs, which is usually the calf or thigh, a dull and heavy ache in the affected area, also flushing warm skin in the area of the clot, visibly red skin at the area below the knee and back of the leg.