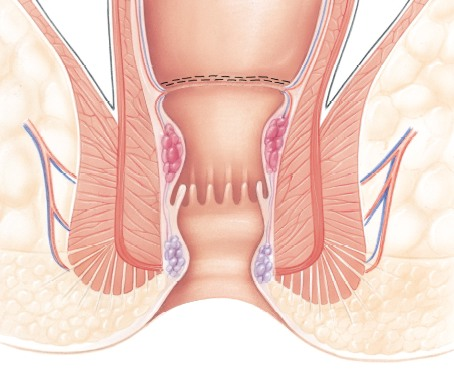
Are you tired of the discomfort and pain that comes with piles? You’re not alone. Many people struggle with this common condition, but there is a natural and effective way to find relief. Fibre, a humble nutrient found in everyday foods, plays a very important role in preventing and managing piles. In this blog, you will learn how adding more fibre to your diet can make a significant difference in your digestive health and overall well-being.
What is the Role of Fibre in Piles?[1]
Fibre adds bulk to the stool and helps it pass more easily through the intestines. There are two types of fibre: soluble and insoluble.
- Soluble fibre dissolves in water and forms a gel-like substance, which slows down digestion.
- Insoluble fibre does not dissolve in water and adds bulk to the stool, aiding in its movement through the digestive tract.
Sources of Dietary Fibre[2]
Incorporating fibre into your diet is simple and can be achieved through a variety of foods. Here are some excellent sources of dietary fibre:
- Fruits: Apples, bananas, oranges, and berries.
- Vegetables: Carrots, broccoli, spinach, and sweet potatoes.
- Whole Grains: Brown rice, oatmeal, and whole wheat bread.
- Legumes: Lentils, beans, and chickpeas.
- Nuts and Seeds: Almonds, chia seeds, and flaxseeds.
Preventing Piles with Fibre[3]
- Regular Bowel Movements: One of the primary benefits of fibre is its ability to promote regular bowel movements. Regular bowel movements prevent the build-up of pressure in the rectal veins, reducing the risk of developing piles. A fibre-rich diet ensures that your digestive system works efficiently, making it less likely for you to experience constipation, a major contributing factor to piles.
- Softens Stool: Fibre helps soften the stool by absorbing water, making it easier to pass. Hard, dry stools can lead to straining during bowel movements, which can cause or worsen piles. By consuming enough fibre, you can maintain soft, easily passable stools, reducing the strain on your rectal veins.
Managing Piles with Fibre[3]
If you are already experiencing piles, making dietary adjustments to include more fibre can help manage the condition. A high-fibre diet can alleviate symptoms such as pain, itching, and bleeding. Here are some tips to increase your fibre intake:
- Start your day with a high-fibre breakfast, such as oatmeal topped with fruits and nuts.
- Include plenty of vegetables in your meals, aiming for a variety of colours and types.
- Snack on fruits, nuts, and seeds instead of processed snacks.
- Choose whole grains over refined grains.
Fibre Supplements
In addition to dietary changes, fibre supplements can be helpful in managing piles. Supplements can provide the necessary fibre intake if you are unable to get enough from your food alone. However, it is always recommended to consult your healthcare provider before consuming these supplements.
Recommended Fibre Intake for Piles
The recommended daily intake of fibre varies depending on age and gender. On average, adult women should aim for about 25 grams of fibre per day, while adult men should aim for about 38 grams[4]. These recommendations can serve as a guideline for adjusting your diet to ensure adequate fibre intake.
Sample High-Fibre Diet Plan[5]
To help you add more fibre into your diet, here’s a sample high-fibre diet plan:
Breakfast:
- Oatmeal cooked with milk, topped with chopped apples, almonds, and a sprinkle of chia seeds.
- A glass of freshly squeezed orange juice.
Mid-Morning Snack:
- A bowl of mixed fruits such as papaya, guava, and pomegranate.
Lunch:
- Brown rice or whole wheat roti.
- A serving of dal (lentil soup) and a vegetable curry made with spinach, carrots, and peas.
- A side salad with cucumbers, tomatoes, and a lemon dressing.
Afternoon Snack:
- A handful of roasted chickpeas or a small bowl of yoghurt with flaxseeds.
Dinner:
- Quinoa or whole wheat pulao.
- A serving of mixed vegetable curry with beans, cauliflower, and sweet potatoes.
- A side of sautéed greens such as spinach or methi (fenugreek leaves).
Before Bed:
- A small bowl of fruit salad or a few pieces of dried figs.
Conclusion
Incorporating more fibre into your diet is a natural and effective way to prevent and manage piles. Start making these changes today to experience the benefits of a healthier, more comfortable life.
Reference Links:
[1] https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983#:~:text=Soluble%20fiber.,%2C%20carrots%2C%20barley%20and%20psyllium.
[3] https://www.news-medical.net/health/Prevention-of-piles-(Haemorrhoids).aspx
[4] https://www.medicinenet.com/how_can_i_eat_25_grams_of_fiber_a_day/article.htm#:~:text=According%20to%20the%20American%20Heart,may%20need%2030%2D38%20grams.
[5] https://www.healthifyme.com/blog/high-fibre-diet/
https://www.lybrate.com/topic/high-fiber-diet
https://www.prevention.com/food-nutrition/a20516445/high-fiber-diet-plan/
https://www.medicalnewstoday.com/articles/hemorrhoids-high-fiber-diet#foods-to-eat
https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/eating-diet-nutrition
https://www.guysandstthomas.nhs.uk/health-information/piles-haemorrhoids/lifestyle-changes#:~:text=Eat%20a%20high%20fibre%20diet&text=Eating%20lots%20of%20high%2Dfibre,muesli%2C%20oats%20and%20bran%20flakes