Introduction
Many people suffer from piles, another term for Haemorrhoids, but the symptoms are always not the same and vary from person to person. These variations mean that not everyone will have the same experience with this common ailment. Therefore, there are varying degrees of severity depending on the presence or absence of symptoms.
What are Haemorrhoids?
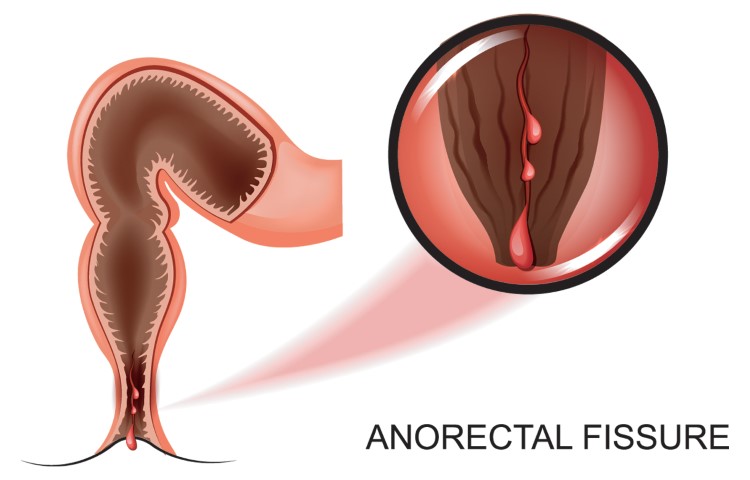
Piles or Haemorrhoids are a widespread disorder that affects the large and/or small blood vessels of the rectum and/or anal canal. They cause localized swelling and painful inflammation of the tissues and veins in the lower anus and rectum, leading to tissue growths varying in and around the anus, leading to significant discomfort. It usually occurs due to straining during bowel movements and sitting on the toilet for long periods. This inflammation can cause bleeding, swelling, and itching, which is why it’s also known as anal fissure or anal itching. Although it can occur at any age, it is more likely to strike after middle age and especially after childbirth. The discomfort resulting from Haemorrhoids can be so intense that some people mistake it for a more serious medical condition such as appendicitis or internal bleeding.
Types of Haemorrhoids
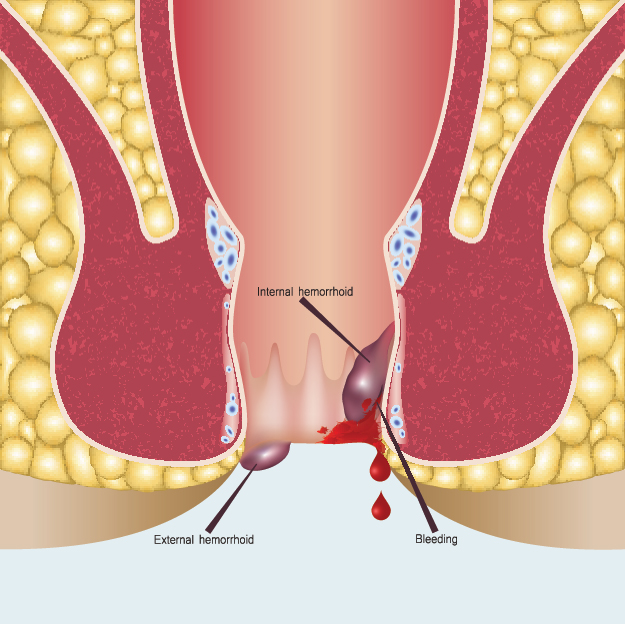
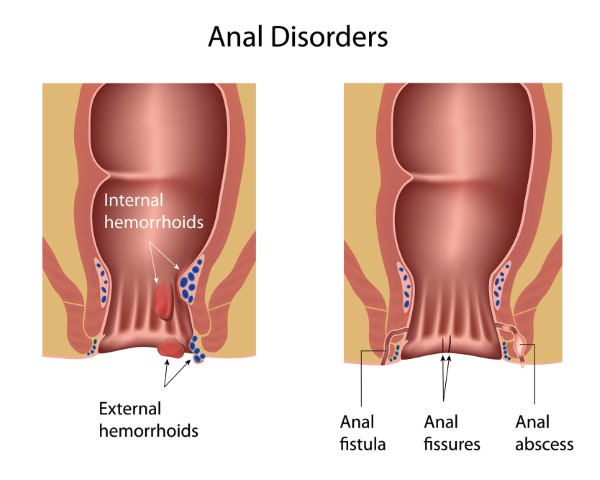
There are two kinds of Haemorrhoids- internal and external.
Internal piles are typically not visible during an external examination and occur within the rectum. In contrast, an external one protrudes outside of the anus forming small lumps around the outside edge, the medical term being prolapsed hemorrhoid. They can be very itchy and painful should a blood clot develop, which can block blood flow. Such thrombosed external piles need immediate medical attention.
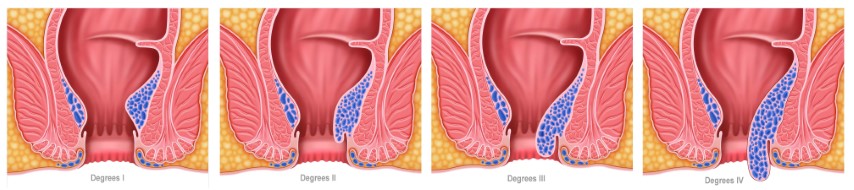
Doctors have graded internal piles as follows,
- Grade 1, where the growth of tissues does not protrude out of the anus and cause any symptoms.
- Grade 2, where the prolapsed Haemorrhoids go back inside on their own.
- Grade 3, where the prolapsed hemorrhoid requires manual intervention to recede.
- Grade 4, the piles prolapse outside of the anus, and manual intervention cannot push it inside.
Causes of Haemorrhoids
Haemorrhoids or piles are a result of increased pressure in the lower rectum, and several factors cause them,
- an anal sphincter (the muscle that controls stool movement),
- weakness and/or spasms,
- sitting too long on the toilet,
- not wiping enough in a sitting position,
- straining during bowel movement
- Chronic diarrhea
- Chronic constipation
- Lifting heavy objects
Diet may also play a role in the development of this condition. Bodies react to certain substances found in certain foods, and sometimes this reaction causes the veins of the anus to become irritated and swollen. A high-fiber diet may increase the risk of developing Haemorrhoids because it increases the amount of stool passed through the body. An increase in fiber in the diet may make it more difficult to fully evacuate the intestines, resulting in straining and, ultimately, Haemorrhoids.
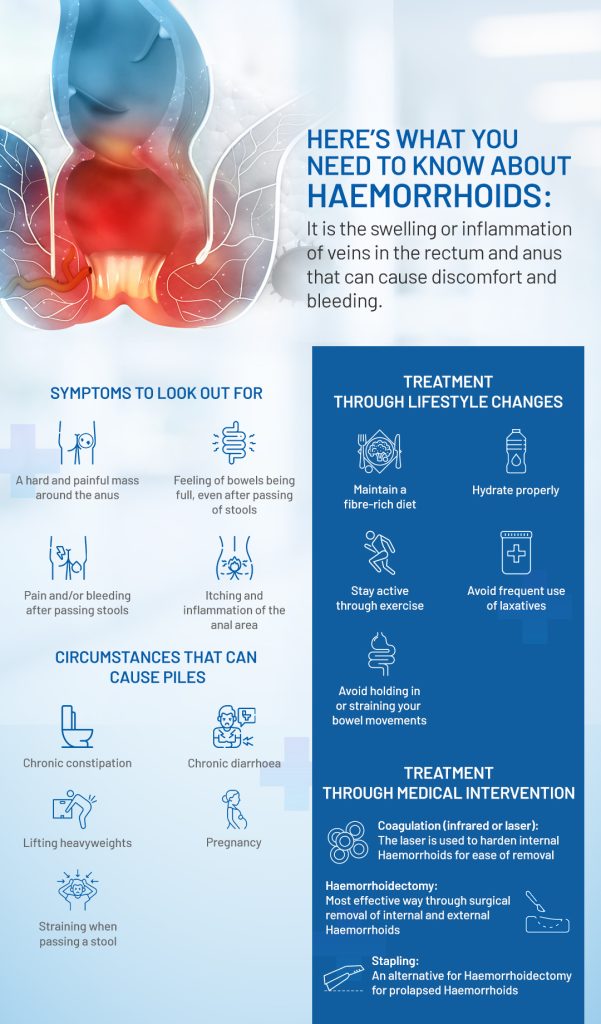
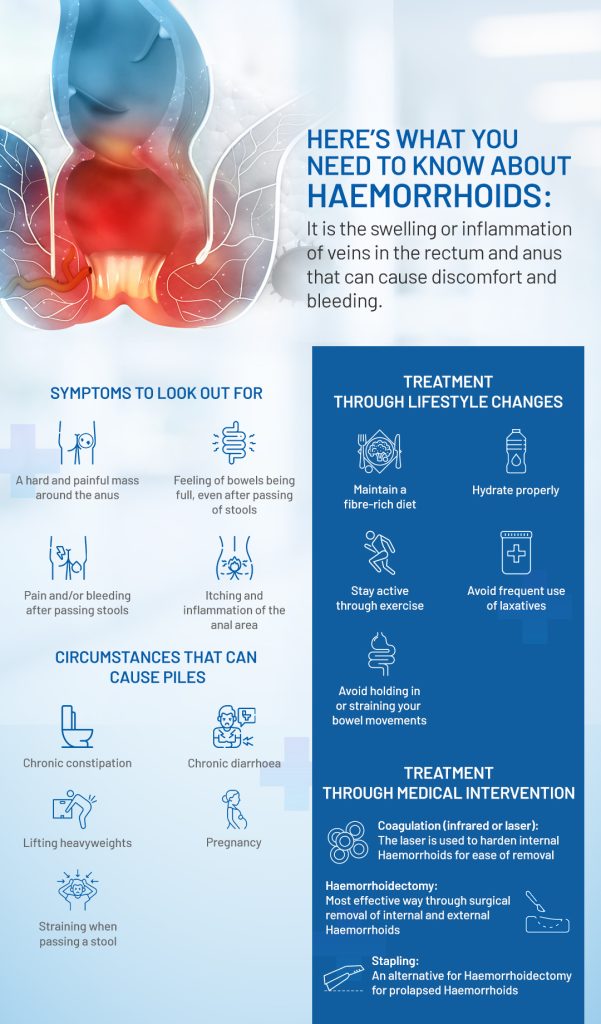
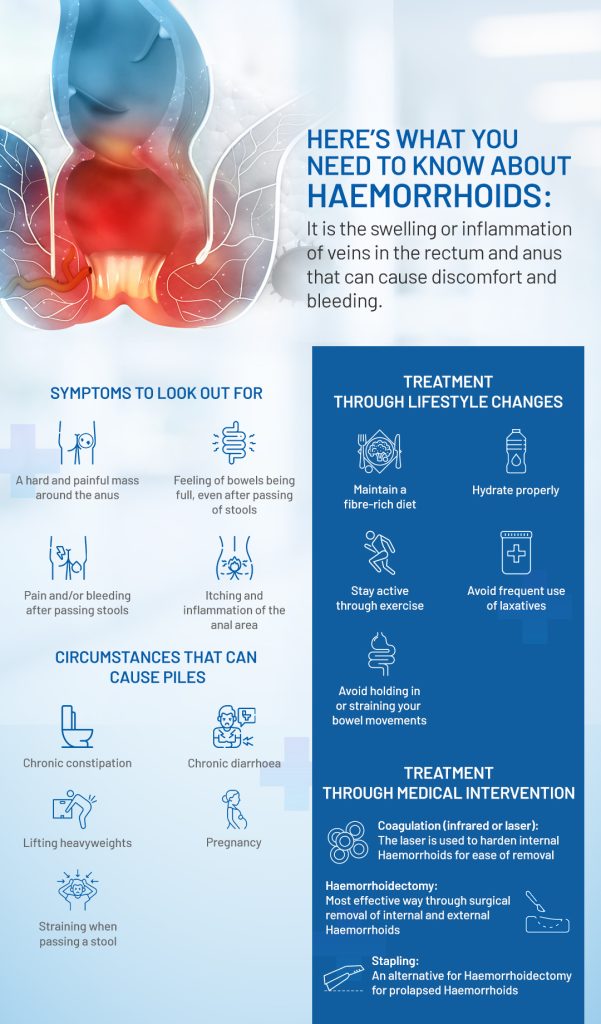
Symptoms of Haemorrhoids
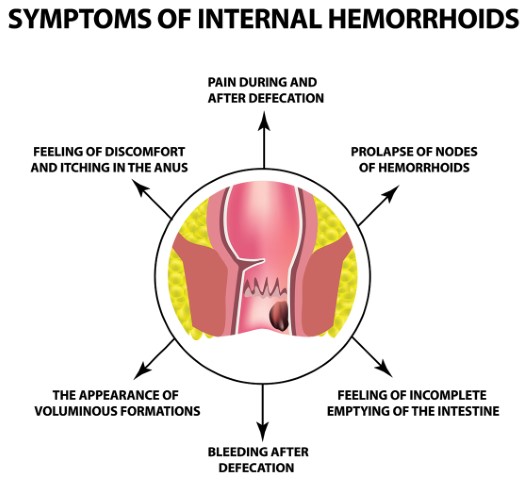
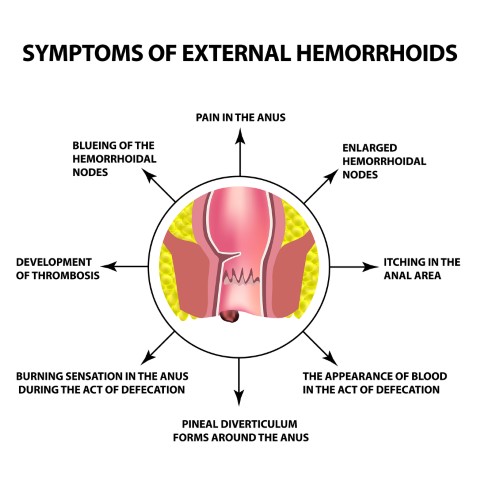
In most cases of piles, the symptoms are not very serious and go away on their own. The most common symptoms experienced are
- Pain. Pain or discomfort in the anus that comes and goes, including lumps. Pain can be mild to severe and can be experienced as a burning sensation, aching, or pressure.
- Bleeding. Haemorrhoids may also cause bleeding or an urgent need to pass stool due to anal spasms. Excessive bleeding can lead to anemia and infection.
- Itching. Itching and discomfort around the anus or rectum.
- Discomfort. Feeling of discomfort during and after passing stools, and/or a feeling of fecal incontinence like one needs to pass stool, but nothing is happening.
- Blood in stools. Blood while passing stools is a common symptom of piles.
Risk factors of Haemorrhoids
Certain factors increase the risk of getting piles like,
- Straining. Straining while having a bowel movement.
- Toilet Overuse. Sitting on the toilet for extended periods.
- Age. The condition is more likely to occur in older individuals.
- Obesity. Overweight people are more likely to develop piles.
- Diet. Haemorrhoids are more likely to occur in people who consume a low-fiber diet.
- Pregnancy. Pregnant women often develop Haemorrhoids because of the increased amount of stool passing through their digestive tracts. In addition, the increased pressure on the veins in the anal canal can cause them to become swollen and painful.
When to See a Doctor
When there is persistent bleeding from the rectum for more than a week, the individual must see a doctor.
Diagnosis
At the time of physical examination of th anus for suspected piles, the doctor will ask the following,
- Family history of piles
- Presence of blood or mucus in the stools
- Color of stool
- Any recent unexplained weight loss
- Any recent change in bowel movement
In case of internal piles, the doctor may use a proctoscope to perform a digital rectal examination (DRE) to see the anal canal up close and collect a tissue sample from inside the rectum for clinical analysis. In addition, the patient may be recommended to undergo colonoscopy if the signs and symptoms indicate a digestive system disease or risk factors for colorectal cancer.
Food to help treat and prevent Haemorrhoids
The following foods help in the management, treatment, and prevention of Haemorrhoids,
- Bananas – This fruit’s high fiber content helps prevent and treat Haemorrhoids.
- Whole-wheat bread – This is a high-fiber bread that helps to prevent and treat Haemorrhoids.
- Oatmeal – This high-fiber food is also rich in essential vitamins and minerals.
- Cucumber – This vegetable is high in water, which helps to keep the anal canal hydrated, reduces inflammation, and prevents and treats anal itching.
- Grapes – This fruit is high in natural antioxidants that have anti-inflammatory properties.
- Apples – Apples’ high fiber content helps prevent and treat Haemorrhoids.
- Kiwi fruit – This high-fiber fruit is rich in vitamins and minerals, which have anti-inflammatory properties.
- Pineapple – This high-fiber fruit is rich in vitamin C and anti-inflammatory properties.
- Watermelon – This high-fiber fruit is also rich in vitamins and minerals.
Prevention and Treatment for Haemorrhoids
In most cases, Haemorrhoids resolve on their own and require no treatment. However, in some cases, medicines and treatment will be given to reduce the pain and discomfort of itching and make the symptoms more manageable.
- Medications – Your doctor may prescribe anal fissure medications. These include over-the-counter (OTC) painkillers, anti-inflammatory agents, and antibiotics to reduce discomfort, stool softeners, and laxatives to soften the stool and make it easier to pass and reduce the pain. These medications are to be taken for a certain period of time and then stopped.
- Antispasmodics and Anal Sterilization – These are herbs or supplements that are to be taken orally or inserted into the anal canal to reduce anal spasms and relieve anal pain. These are non-prescription remedies that are to be taken for a certain period of time until the condition goes away.
- Ointments – Corticosteroid creams and anal fissure ointments help to relieve itching and reduce inflammation and pain.
- Home Remedies – Some people prefer to use natural remedies to treat their Haemorrhoids. These include eating cucumbers and drinking watermelon juice.
- Lifestyle Changes – Doctors will recommend a bunch of lifestyle changes to manage and lower the risk of developing Haemorrhoids. Those measures include regular exercise to stay active, maintaining moderate weight, avoiding heavy lifting and caffeinated drinks, increased water intake and food high in fiber to prevent constipation, and not straining while going to the bathroom.
- Natural Remedies – Haemorrhoids can be a source of great discomfort. If this is the case, talk to your doctor about the possibility of using natural remedies to reduce the pain and treat the condition.
Procedural Options
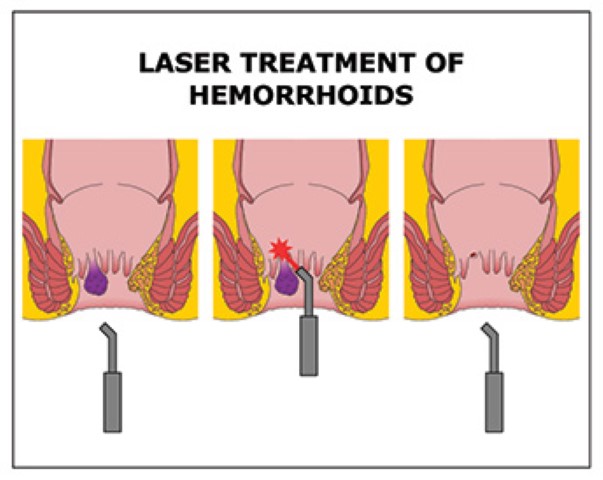
There are minimally invasive procedures should medications and home treatments fail to treat piles or in case of severe prolapsed piles or heavily bleeding internal piles.
- Rubber Band Litigation: Employed to treat prolapsed piles, the doctor wraps a specific type of elastic band around the base of the Haemorrhoids, cutting off its blood supply. The banded component of hemorrhoid shrivels and falls off within a week.
- Sclerotherapy – Especially effective for Grade 2 and Grade 3 Haemorrhoids, the doctor injects a medicine into the Haemorrhoids causing them to shrink and stop bleeding.
- Infrared Coagulation – In this procedure, the doctor uses an infrared light devise to burn the tissues of the internal piles. As a result, scar tissues form, cutting off the blood supply and reducing the piles.
- Hemorrhoidectomy: Hemorrhoidectomy as a surgical procedure involves complete removal of the prolapse of Haemorrhoids. There is always the risk of complications like difficulty in passing stools.
- MIPH (Minimally invasive procedure for Hemorrhoid): In this procedure, the internal hemorrhoid tissue is removed, and the doctor will pull back the prolapse of internal hemorrhoid into the anus by using a special stapling circular device and cut off the blood supply to the hemorrhoid tissue.
FAQs
Haemorrhoids may go away on their own if the underlying risk factors are addressed, such as straining while having a bowel movement and not sitting on the toilet for too long.
Regular exercise, a high fiber diet, and drinking plenty of water can help prevent and treat Haemorrhoids.
Some people prefer to use natural remedies such as nettle leaf, aloe vera, and honey to treat their Haemorrhoids.
Haemorrhoids are common, but not every individual experiences pain or discomfort.
See a doctor if you experience any pain or discomfort during a bowel movement.
If left untreated, piles can be severe and debilitating, affecting one’s quality of life.
If you experience pain at the time of passing stools and see blood in the stools, that is an indication of piles.