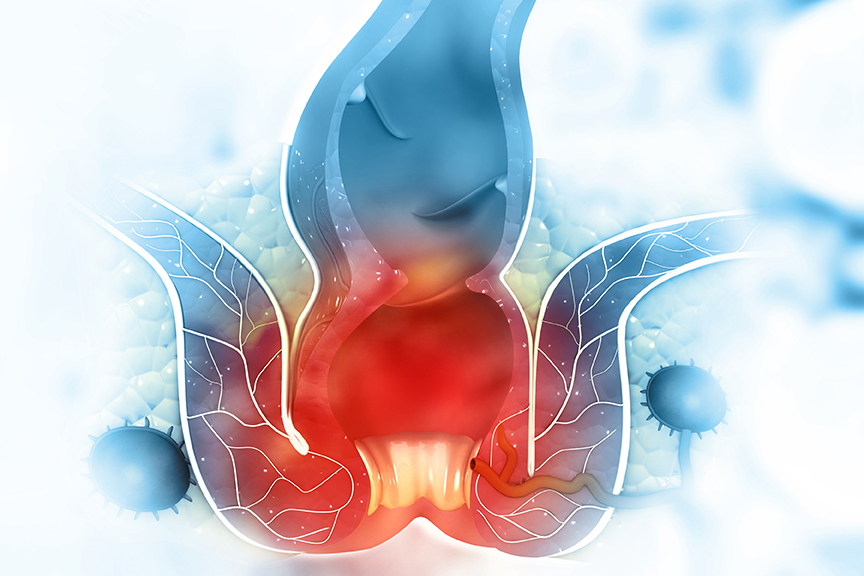
Hemorrhoids, usually known as piles, are caused due to swollen veins around the anus or in the lower rectum. Every year, almost 10 million people in India suffer from this disease due to numerous factors such as stress, insomnia, constipation, and a growing inclination towards fast food. Studies suggest that every second individual in this world experience piles between the age of 45-60 and many women experiences it during their pregnancy.
Some of the symptoms to diagnose piles include extreme itching, irritation, painful bowel movements, and blood in stools. Although the risk factors are still not determined, some of them may include straining during a bowel movement, complications from chronic constipation, and sitting for a longer period. Hemorrhoids can also be passed on genetically, so if you have a family history of piles, it’s most likely that you may develop them too.
Diet plays a vital role in treatment of piles; people who consistently consume a fibre rich diet are less likely to get the disease than the ones blindly following the junk food culture. The studies suggest that people these days need to inculcate good food habits to combat problems like hemorrhoids.



If you’re experiencing extreme pain or any of the symptoms mentioned above, then consulting your primary physician must be the first step. Your doctor generally can diagnose piles during routine physical examination. The doctor will check the area around your anus for
- lumps or swelling,
- internal hemorrhoids that have fallen through your anal opening, called prolapse
- external hemorrhoids with a blood clot in a vein
- anal fissures—a small tear in the anus that may cause itching, pain, or bleeding
- Leakage of stool or mucus
- Skin irritation etc.
The doctor will perform a digital rectal exam to examine external hemorrhoids, however, diagnosing internal piles may include an examination of your anal canal and rectum. Doctor examines your anus through a tube fitted with a light at its end, called a proctoscope. An endoscopy can also be recommended for a detailed evaluation and to rule out any other digestive tract disorders.
Piles may not show symptoms in many individuals at all times. You can often alleviate the mild pain and inflammation of hemorrhoids with home remedies. If detected at an early stage, it can be cured with just medication and simple lifestyle changes. However, if the symptoms are severe and pain is unbearable, the following medical treatment options for piles can assist you in curing them.
- In majority of the cases, it resolve on their own. However, some anti-itching topical agents can significantly minimize the discomfort in patients.
- Several OTC (Over-the-counter) products, such as painkillers and topical anti-inflammatory agents can help in minimizing redness and swelling surrounding the anus.
- Taking laxatives (substances that loosen stools and increase bowel movements), upon doctor’s advice can help a patient with constipation for easy defecation.
- In the later stages, surgery is a must and there are various surgical procedures available for the treatment of piles.
As mentioned above, some of the home remedies for the treatment of piles include eating high fibre foods such as fruits, vegetables, and whole grains, using topical treatments, and doing regular pelvic floor exercises. For continuous bleeding or painful hemorrhoids, your surgeon might advise other minimally invasive procedures available. Although only a small section of individuals suffering piles require surgery if any other procedure hasn’t been successful, your surgeon may recommend one of the following:
- Haemorrhoid removal: In this procedure, you will be given general anaesthesia to combat pain. Incisions are made in the tissue surrounding the haemorrhoid. Then the swollen vein is tied off to prevent bleeding and the haemorrhoid is removed.
- Haemorrhoid stapling: This procedure is used to treat prolapsed hemorrhoids. A surgical staple fixes the prolapsed haemorrhoid back inside your rectum while cutting off the blood supply so that the tissue will shrink and be reabsorbed. Stapling recovery takes less time and is less painful than recovery from a hemorrhoidectomy.



Summing up, taking utmost care of yourself post-surgery should be your priority. Maintaining a healthy lifestyle including a balanced diet is paramount. Though you can expect some pain post a haemorrhoid surgery too but with proper treatment and following all the necessary doctor guidelines will gradually reduce the impact of the pain on your road to recovery. On the other hand, if you haven’t diagnosed piles yet then it is important to know that Hemorrhoids don’t always come with symptoms, so you may not realize you have them but in case you start experiencing any discomfort like itching or difficulty in passing stool and your personal attempts to treat them don’t show positive results then it’s better to let your doctor know.