Say No to Myths
Separating facts from fiction is the first step towards creating awareness about any disease for advancing its prevention, timely diagnosis, and treatment. Myths, as misconceived, misinformed, false, or misleading information about any medical condition, are barriers to achieving the much-needed medical intervention and controlling the spread of diseases. Debunking such myths helps-
- Promote awareness and correct information and knowledge about diseases and
- Curtail the aggravation of the condition and prolongation of the associated discomfort, pain, and agony arising through proper and timely treatment.
This blog discusses a common disease of sinus inflammation, known as Sinusitis and some of the sinus misconceptions that need to be debunked.
Understanding Sinus Health
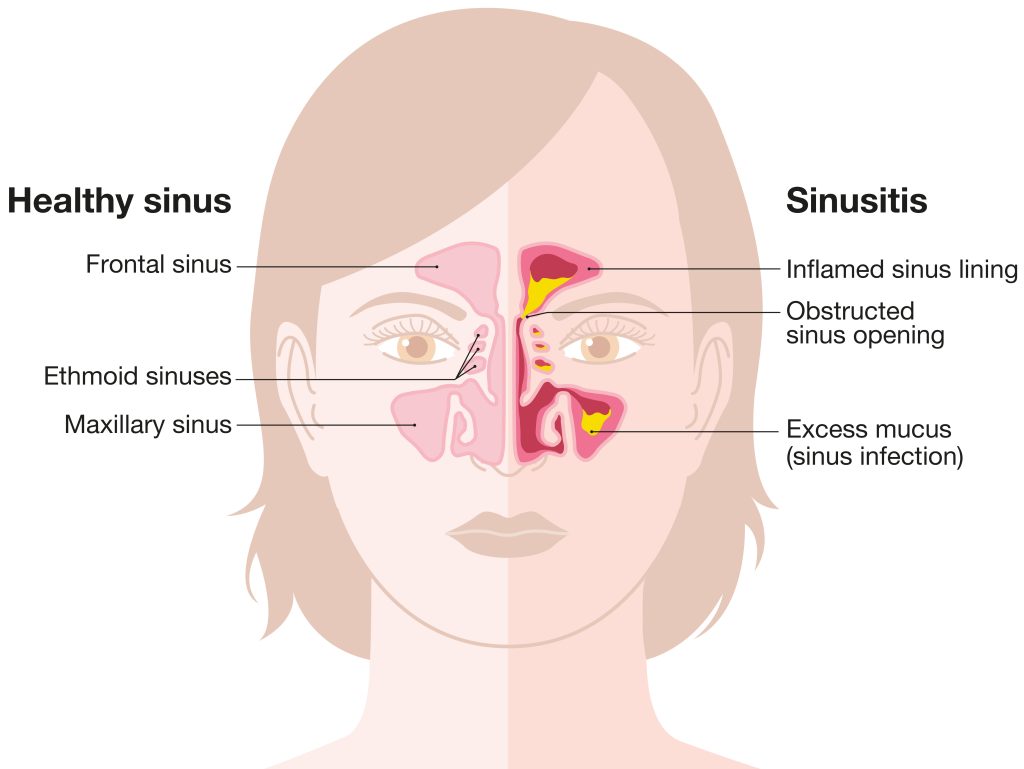
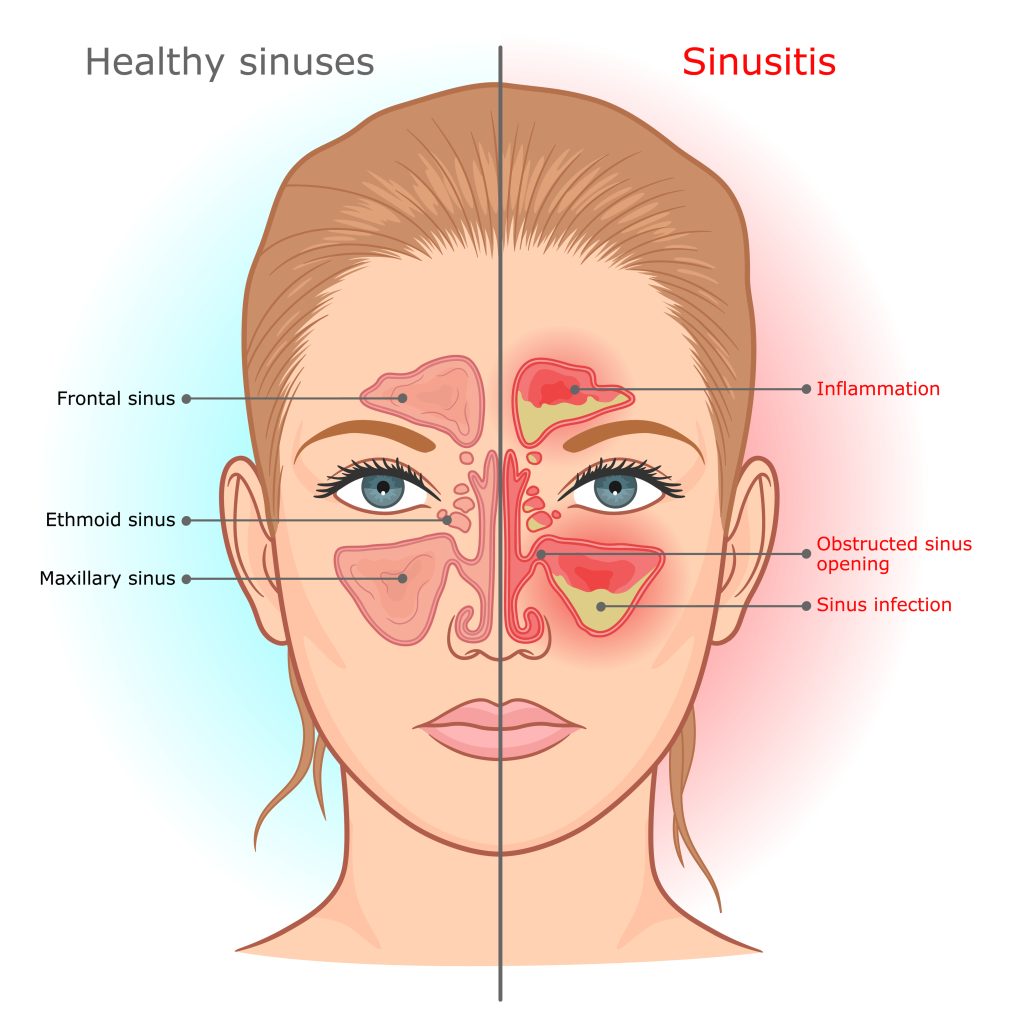
Sinusitis is a condition of inflammation of the tissue lining in the sinus (cavities or spaces in the forehead, nose, and cheeks that are filled with air). Common colds, virus or bacterial infections, fungi, or allergies cause blockage in the sinuses that get filled with fluid. The pressure of these blocked fluids causes pain in the forehead, face, and nasal congestion.
- Types of sinus infection- Depending on the duration and severity of the infection, it may be Acute (lasts for four weeks or less), Subacute (lasts between four to twelve weeks), Chronic (lasts for a minimum of twelve weeks), or Recurrent (comes and goes four times a year and lasts for less than two weeks each time).
- Symptoms – Some common symptoms are stuffy or runny nose, toothache, pressure or pain on the face, cough, fever, headache, or fatigue.
- Risk factors- People with allergies, asthma, polyps, nasal structural deformity, and weak immune systems are at a higher risk of having this infection.
- Treatment- The treatment and medication (decongestants, pain relievers, intranasal steroids) depend on the type of sinus infection. However, home remedies (humidifiers or vaporizers, steam inhalation, saline nasal spray, warm compress application, or plenty of fluid intake) are the first preference for treating sinusitis. In severe cases, surgery may be recommended.
Sinus surgery treats the disease, relieving symptoms, and related discomfort by removing the blockages and opening the air pathway. The surgery removes nasal polyps, tiny bones, diseased tissue, or tumor growth, blocking the nasal passage. The surgeries to treat sinusitis are-
- Functional Endoscopy Sinus Surgery (FESS): Using an endoscope, an otolaryngologist examines the inside of the nose and sinuses and accordingly conducts the surgery to remove the polyp, bone, or tissue obstructing the drainage of the mucus.
- Sinus Balloon Dilation Procedure: This minimally invasive procedure uses an endoscope and a catheter to guide a balloon to the site of nasal blockage. The balloon at the tip of the catheter is inflated, opening the blocked nasal passage.
- Turbinate Reduction Surgery: Turbinate is a tiny structure in the nose that cleanses the air passing through the nostrils. The surgery reduces the size of the turbinate using a needle-like instrument, thus making space in the nasal passage.
Myths and Facts
The treatment for sinusitis requires awareness of the condition, including but not limited to the causes, symptoms, risks, types, different treatment options, post-operative care, and recovery. Any misconception or misinformation about the condition may hamper its timely treatment and aggravate it. To this end, one must not buy into any myths surrounding the disease. Some of the common myths relating to the disease are-
Myth- Sinusitis is contagious.
Fact- It is not contagious. It is not a communicable disease, but if one gets a viral infection, it can lead to sinusitis.
Myth- Antibiotic is a must for sinusitis.
Fact- Every type of sinus infection does not require an antibiotic. The need for an antibiotic depends on the severity and duration of the condition. Generally, it can be managed by home remedies, rest, nasal spray, or pain medication. Antibiotics are prescribed if the condition does not improve for a week or more.
Myth- Sinusitis can resolve on its own.
Fact- Though a common condition like a common cold, sinusitis requires proper treatment and attention through home remedial measures, medications, and, in chronic or recurrent cases, when these do not work, through surgery.
Myth- Green or yellow mucus is a sign of bacterial infection.
Fact- Green or yellow mucus may be due to the death of infection-fighting white blood cells. It is not the colour but the duration of this mucus drainage that indicates whether it is a sinus or bacterial infection.
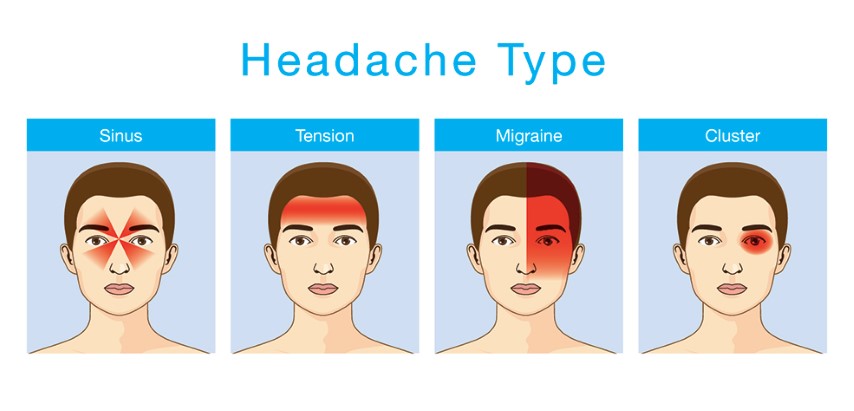
Myth- Headaches in the sinus areas are caused by sinus infection.
Fact- Sinus headaches may result from common colds, migraines, allergies, or other neurological conditions.
Myth- Decongestant spray cures breathing problems.
Fact- Decongestant spray temporarily relieves stuffy nose but does not permanently cure breathing. Long-term use of these sprays adversely affects the heart and may lead to other health problems.
Conclusion
Sinusitis, though a common health problem, needs proper attention and care to avoid its aggravation and further complications. It can be managed with home remedies, medications, and, in severe cases, through surgery. Stay away from misleading information and avoid basing your medical decision on myths. It is always wise to stay informed, aware, and updated with the correct information and knowledge about one’s health and related treatment therapies. The right information empowers the right decision.
References
https://houstonadvancedsinus.com/debunking-5-common-myths-about-sinusitis/#:~:text=Myth%202%3A%20%E2%80%9CAll%20Sinus%20headaches%20are%20caused%20by%20sinusitis.%E2%80%9D&text=Common%20cold%20at%20times%20may,lead%20to%20bacterial%20sinus%20infection.&text=Migraine%20attacks%20are%20one%20of,that%20result%20in%20sinus%20headaches.
https://www.healthshots.com/preventive-care/self-care/common-sinus-myths/
https://www.indiatvnews.com/health/here-are-some-common-sinus-myths-you-shouldnt-believe-get-your-facts-correct-latest-health-news-2023-02-21-849197