Hemorrhoids are one of the most common anorectal disorders; according to NCBI it affects around 25% to 30% of the population. People of all ages, genders, races, and ethnicities are affected. Piles become increasingly common as people become older, affecting more than half of those over the age of 50. Hemorrhoids are very common, so don’t be shy to get help! Hemorrhoids are bulging, inflated veins that occur in the anus and rectum (Back passage). They can be unpleasant, painful, and cause rectal bleeding. Hemorrhoids, are natural cushions we’re all are born with, although they don’t bother us at first. They only cause uncomfortable symptoms when they become swollen and enlarged, then known as swollen piles.
Hemorrhoids (Piles) are a topic that most people avoid discussing and prefer being silent about. But being silent may prevent you from receiving treatment for a common ailment and which can land you up in severity. Your doctor isn’t shy about bringing up the subject of haemorrhoids, so discuss freely.
When to see the doctor?



Most people think of hemorrhoids as a minor problem, it can be very painful. It is important to know when to treat hemorrhoids on your own and when to seek help, as it can avoid unnecessary complications.
Make an appointment with your doctor if you’re having any of the following symptoms related to your hemorrhoids:
- You notice bright red blood on your toilet paper or have rectal bleeding.
- Your rectum or anus is causing you agony and discomfort.
- You’ve tried over-the-counter medications for more than a week and they haven’t helped you.
- You experience a maroon or dark tar-colored bowel movement, which could be an indication of bleeding.
- You feel mass outside your back passage
If your rectal bleeding won’t stop and you’re feeling dizzy or faint, it’s a medical emergency that necessitates a visit to the Emergency room (ER).
How do doctors treat Haemorrhoids?
Hemorrhoids are treated by doctors in the office, in an outpatient clinic, or a hospital. Treatment depends on severity. For an initial stage of piles lifestyle changes can help you if given at on right time. For mild piles office procedures can help you. But for severe piles surgery is the only option.
Office procedures for very mild piles:
- Rubber band ligation: Rubber band ligation is a treatment that surgeons employ to treat internal hemorrhoids that are bleeding or prolapsing. A doctor wraps a specific type of rubber band around haemorrhoid’s base. The band stops the blood supply. Within a week, the banded component of hemorrhoid shrivels and slumps.
- Sclerotherapy: In this therapy, a surgeon injects a special chemical into haemorrhoids, which causes the haemorrhoid to shrink, while also stopping it from bleeding.
- Photocoagulation with infrared light: A doctor employs an infrared light instrument to treat internal hemorrhoids. Scar tissue forms as a result of the infrared light’s heat, cutting off the blood supply and reducing hemorrhoids.
- Electrocoagulation: A doctor inserts an electric current into an internal hemorrhoid with an instrument. Scar tissue forms as a result of the electric current, cutting off the blood supply and reducing hemorrhoids.
Surgical procedures for moderate to severe piles:
- Haemorrhoidectomy: A haemorrhoidectomy is a procedure in which a surgeon removes the prolapse of hemorrhoids (which is coming out from the back opening) by cutting it directly with a scalpel, scissors, or electrical energy source.
- MIPH (Minimally invasive procedure for Hemorrhoid): Internal hemorrhoid tissue is removed and the prolapse of the internal hemorrhoid is pulled back into the anus by using a special stapling circular device.
Today, let us know more about MIPH
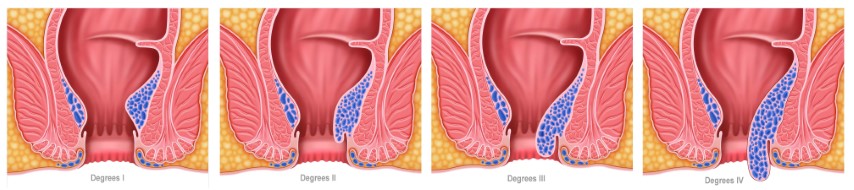
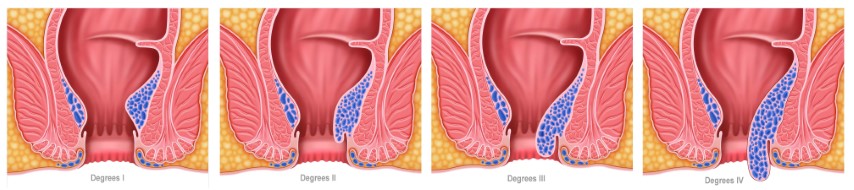
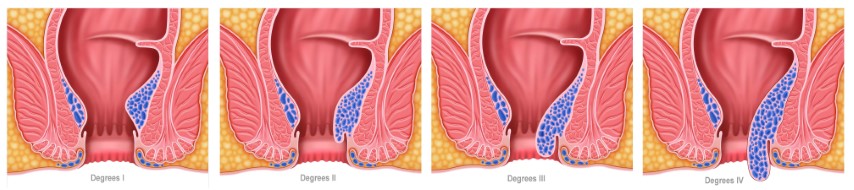
MIPH (Minimally invasive procedure for Hemorrhoid) or Stapled haemorrhoidopexy is a surgical procedure for treating hemorrhoids. It is the preferred therapy for third and fourth-degree hemorrhoids (a severe form of piles that protrude with straining and are visible on physical examination outside the anal margin. The manual reduction must be done on a regular or irregular basis). Stapled haemorrhoidectomy is a misnomer because the procedure removes the unusually slack and enlarged tissue which supports hemorrhoids that have caused the hemorrhoids to prolapse downward, rather than the hemorrhoids themselves.
A circular, short hollow tube is introduced into the anal canal for stapled haemorrhoidopexy. A suture (a long thread) is woven circumferentially through the anal canal above the internal hemorrhoids through this tube. The stapler (a disposable instrument with a circular stapling device at the end) is inserted into the hollow tube, and the suture ends are brought together and pulled inside the stapler along with prolapsed hemorrhoids. Stapler when fired causes cutting of slack tissue and stapling of hemorrhoids back to their original position.
Patients who undergo a minimally invasive procedure for hemorrhoids (MIPH)/ Stapled Haemorrhoidopexy benefit from the following:
- Return to work as soon as possible
- There is very little discomfort
- There are no cuts, hence there are no dressings required
- There are no follow-ups
- Released from the hospital in a day
Comparison between MIPH and Conventional Haemorrhoidectomy
Haemorrhoidectomy is a procedure that removes hemorrhoids from the body. You will be given general or spinal anesthesia to prevent you from feeling discomfort. Around hemorrhoids, incisions are made in the tissue. To prevent bleeding, the enlarged vein inside the hemorrhoid is tied off, and the hemorrhoid is removed. It is possible to suture the surgical area to shut it or leave it exposed. The wound is covered with medicated gauze. A knife (scalpel), an electric tool (cautery pencil), or a laser can be used to do surgery. In most cases, the procedure is performed in a surgical center. You’ll probably return home the next day or more.
Stapler Haemorrhoidectomy / MIPH (Minimally Invasive Procedure for PILES) is a procedure where an expert surgeon employs stapling equipment to remove a portion of the pile mass with a staple gun, addressing two major concerns: bleeding and prolapsed hemorrhoids. The titanium staples not only cut but also seal at the same time, which lowers bleeding and post-operative pain. Because no extra incision on the lower region of the anal canal is necessary, the patient does not require any post-operative dressing. A patient can return home the same day and resume normal life in a day or two.
The most prevalent complaints of piles are painless rectum bleeding and haemorrhoidal prolapse, painful defecation. When compared to open haemorrhoidectomy, the average length of surgery for MIPH and post-operative bleeding is much shorter. The postoperative pain score and subsequent need for analgesics are significantly lower in the MIPH. MIPH patients have a faster average wound healing time and a quicker return to routine activities. Less recurrence or incontinence is observed. Similarly, there are no significant differences in long-term problems between MIPH and traditional open haemorrhoidectomy in patients with MIPH.
MIPH is a frequently used and safe procedure for grade III and IV hemorrhoids. It results in less pain, a shorter hospital stay, and fewer early postoperative problems. Wound healing and return to normal activities are faster, and long-term problems are not significantly different.





Comments are closed.