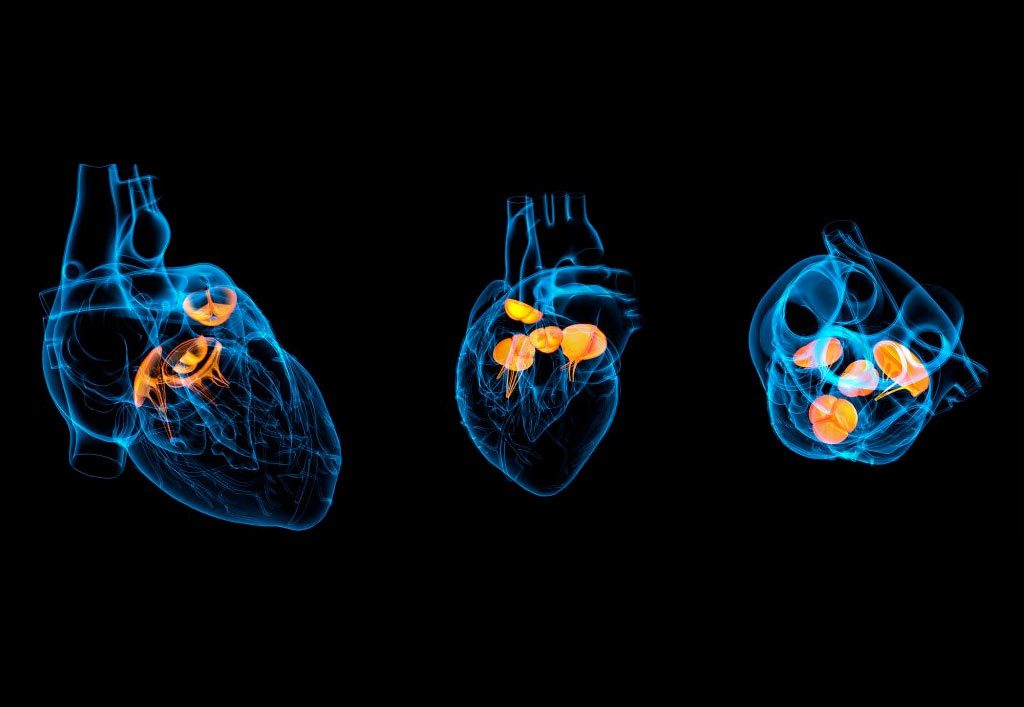
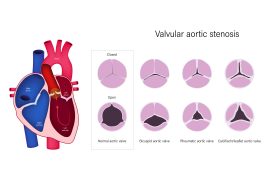
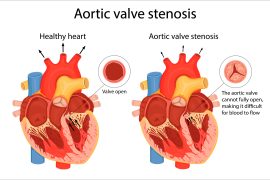
The word aortic stenosis may seem alien, but the condition is one of the most common valvular heart diseases in the world. Usually seen in the elderly, with symptoms surfacing mostly after the age of sixty, Aortic stenosis may also be a congenital condition. Our heart contains four valves, the mitral, tricuspid, pulmonary and the aortic. The former two control the flow of blood from one chamber to another while the pulmonary and aortic direct the blood away from the heart. The pulmonary artery directs the blood to the lungs and the aortic artery directs the blood to the rest of the body. In this condition, an aortic valve begins to show signs of stenosis or narrowing, thus reducing its operating capacity. This results in a reduced supply of oxygenated blood to the body which leads to symptoms like breathlessness, chest pain, fainting and palpitations. If the symptoms are mild or not present, the cardiologist may decide to simply monitor and follow up. However, if the stenosis has shown significant progress and has started to exhibit major symptoms, then the best option is to undergo Transcatheter Aortic Valve Replacement (TAVR).
TAVR is a minimally invasive surgery, as in, the chest bones are not opened up as in a bypass. It is instead a lot like a stent placement procedure. Small incisions are made in one’s groin to access the femoral artery and a hollow tube is placed in it. The new valve is placed on a tube with a balloon tip on one end and crimped to fit the hollow tube. The hollow tube is then inserted into the femoral artery and pushed through until it reaches the diseased valve. At this point, the balloon is inflated which in turn expands the new valve and helps it take its place. The new valve pushes the leaflets of the original valve to secure its place. Once the new valve is up and running, the balloon is deflated and removed.
Transcatheter Aortic Valve Replacement is relatively new. As a result, it is advised only for high and immediate risk patients by regulatory authorities and has shown promise in treating patients at low risk too. As shown by extensive research, heart valve replacement is a safe and suitable option for elderly patients, with recent studies demonstrating a 94% [1] [2] survival rate in 5 years. The survival rate for any individual patient also depends on other factors like their overall and cardiac health, co-morbid medical conditions and age. While early TAVR procedures demonstrated success rates of merely 70-80%, advanced cardiac care, surgical technologies and tools have increased the rates to as high as 92%. The overall procedure is also deemed to be nominally risky with a 2% chance of complications and fatalities across all age groups. This holds true even for elderly patients above 80.
The recovery process for Transcatheter Aortic Valve Replacement can take quite a few weeks. Most cardiologists recommend a course of blood thinners to prevent clots and antibiotics to prevent infection for their patient’s optimum recovery. Patients can expect to resume their normal activities gradually once they are totally recovered but will still have to undergo regular check-ups from their cardiologist. These check-ups are vital as they are meant to ensure that the patient’s heart and new valve are working properly.



When it comes to one’s heart, any risk is too big to take. For those whose lives have been restricted by aortic stenosis, Transcatheter Aortic Valve Replacement therapy provides an opportunity to lead a normal life with normal activities again. With experienced surgeons, advanced tools and techniques, this minimally invasive surgery is sure to change the lives of those who are suffering from the advanced stages of the disease.